Prior to 2020, the Lung Health Foundation operated as the Ontario Lung Association. Enjoy this content from our archives.

An official publication of the Ontario Respiratory Care Society, a section of the Lung Health Foundation
Update Ontario Respiratory Care Society
Update on Respiratory Health, Research and Education is a publication of the Ontario Respiratory Care Society, a section of the Lung Health Foundation. Update is published three times per year and includes peer-reviewed original articles, clinical practice tools, health news, and communications between the ORCS and its membership.

CHAIR’S MESSAGE – Winter 2019
Happy New Year! It really is hard to believe that another year has gone by. And, with this year’s passing, my second year as Chair of the ORCS has gone by completing my term. It’s been a busy two years. Some milestones we’ve achieved together include the re-alignment of some of the regional planning committees to more closely match the Lung Health Foundation regions; the evolution of this electronic publication from two former hard copy newsletters, Update and Connections; and the launch of the membership portal that streamlines membership management, communications and event registration.
This past fall, the ORCS Regional Planning Committees planned and executed five educational events across the province. Topics included: COPD Management, The Effects of Tai Chi in Patients with COPD, From Hospital to Home: Discharge Planning, Long Term Ventilation Clinic Success Stories, and many more. While all events were well received, the Western region committee and local staff had particular success by tapping into the Fanshawe College student body, generating an attendance of more than 90 individuals.
Better Breathing 2019 is almost upon us (Jan 24 – 26, 2019). Canada’s premier respiratory conference caters to those who work in a variety of health-care disciplines including respiratory therapists, nurses, physiotherapists, occupational therapists, social workers, pharmacists, dietitians, and others involved in various aspects of respiratory care. This year’s line-up includes sessions on Genetic Determinants of Lung Disease, Stem Cell-Based Therapies for Lung Diseases, Transitions in Home Mechanical Ventilation and a debate on Motivational Interviewing vs Brief Intervention featuring our own long-time ORCS members, Lana Biro and Ana MacPherson. For more information, or to register if you haven’t already done so, please visit www.BetterBreathing.ca.
And finally, if you like to party, we have the event for you! It’s the 10th anniversary of the Breathe! Gala. Historically held in January on the Thursday evening of Better Breathing, the newly named Breathe! Bash has been moved to March 28. It will be an evening to celebrate, to be inspired and to have fun. The new format will be more conducive to networking and feature a variety of food stations and fun, live entertainment. It’s a night you won’t want to miss! Buy your tickets at: http://support.on.lung.ca/site/PageServer?pagename=Breathe_Gala_Home
While it’s bittersweet to say goodbye, I’m very happy to hand over the reins to your new Chair, the very capable Miriam Freymond Turnbull. Miriam has been working in the respiratory field for 37 years, and has been an ORCS member since the mid 80’s. With a passion for the profession of respiratory therapy, Miriam’s career spans acute and community care, with the most recent 25 years being in various leadership roles in community respiratory therapy.
On a personal level, I have left my position at the University and joined McMaster as Vice Dean (Heath Sciences) and Executive Director School for Rehab Sciences. I am very excited about the opportunity.
I am always available to discuss any comments or suggestions that you may have. Feel free to contact me by email dina.brooks@utoronto.ca or by phone 416-978-1739.
Respectfully submitted,
Dina Brooks, BScPT, MSc, PhD
Chair, Ontario Respiratory Care Society.

EDITOR’S MESSAGE
As respiratory health professionals, an important part of our job is education. Not only the education of patients, ourselves, and our colleagues, but also the education of future health care professionals. It is so satisfying to work with students and to see that glimmer in their eyes when they are truly inspired and interested in learning, particularly in the field of respiratory health and wellness. As busy clinicians, working with students is very rewarding but can also be a hard job at times. We encourage all health professionals to continue to accept this important challenge of educating our future colleagues and hope that some of the articles in this winter 2019 edition of Update on Respiratory Health, Research, and Education will inspire you to continue this work.
Larry Jackson’s BScPhm feature article on Strategies Health Professional Students Can Use to Ensure Success in an Experiential Placement is a very helpful and informative article for both students and preceptors. It outlines how students can get the most out of placement but also guides the “teachers” on how to assist their students in being enthused and ready for a clinical placement.
A comprehensive and well written review of the article Human Airway Branch Variation and Chronic Obstructive Pulmonary Disease by Kayla Kok, a Fanshawe College student, is also featured. It is always encouraging to see students, who are still in training, interested in reviewing current research and sharing their work with us.
The Eye On article features a pulmonary rehabilitation program run by Tammy Draper RRT in North Bay which encompasses education for people with COPD and their families, as well as exercise at a local gym. Theresa Hawn BScPT is the focus of In the Spotlight. As always, included are reviews of Respiratory Articles of Interest which cover self-management of patients with COPD in primary care, the use of Dupilumab in asthma, and smoking cessation.
What better way to further your own knowledge and bring new and exciting ideas back to your own place of work than attending Better Breathing 2019, January 24 to 26, 2019, at the Toronto Marriott Downtown Eaton Centre. Attend for one day or all three days. We hope to see you all there!
Sincerely,
Lorelei Samis PT
Co-chair Editorial Board
Co-chair RHEIG Executive Team

BBC 2019
The Lung Health Foundation invites you to our 36th annual Better Breathing Conference running from January 24-26, 2019 at the Toronto Marriott Downtown Eaton Centre.
Take advantage of this unique opportunity to participate in a range of innovative sessions headed by leading medical professionals. Learn about new approaches to respiratory health, updates on critical research projects and relevant case studies. Over the course of the conference, you will gain exclusive access to more than 25 dynamic sessions, engage with industry-leading experts and network with 300 of your peers in the respiratory field.
January 24 – 26, 2019
RESEARCH AND FELLOWSHIP AWARDS
ORCS Research and Fellowship Committee Chair, Mika Nonoyama, PhD, Assistant Professor, Registered Respiratory Therapist
Research Grants and Fellowship Awards support research and graduate study by health-care providers in the field of respiratory care. The objective of this fund is to promote research regarding any field of acute or chronic lung disease. Research may include investigation of any phenomenon pertinent to illness assessment, management, or responses of the individual with a respiratory condition. Research may also be aimed at health promotion, education and prevention issues. Studies may use quantitative or qualitative methodologies.
The Lung Health Foundation is committed to supporting the best respiratory research in Ontario. The Lung Health Foundation has established focus areas: asthma, air quality and smoking-related lung disease. Projects in these areas are encouraged. However, the primary criterion for the awarding of research monies shall be the excellence of the research proposal.

Strategies Health Professional Students Can Use to Ensure Success in an Experiential Placement
ORCS Research and Fellowship Committee Chair, Mika Nonoyama, PhD, Assistant Professor, Registered Respiratory Therapist
Lawrence Jackson provides advice to help health professional students ensure success in an experiential placement.
Submitted by: Lawrence D. Jackson, BScPhm, Pharmacy Clinical Coordinator, Veterans Centre, Sunnybrook Health Sciences Centre and Adjunct Professor, Leslie Dan Faculty of Pharmacy, University of Toronto
Editor’s note: this article is excerpted from an article titled: Strategies Pharmacy students can use to ensure success in an experiential placement, and has been submitted to Update on Respiratory Health, Research & Education by the original author. The citation for the original article is: Jackson LD. Canadian Pharmacists Journal 2015;148(6):308-313.
Students of the health professions look forward to and value their experiential placements (clinical rotations). The twenty strategies provided in this opinion piece were originally directed at pharmacy students to help them take responsibility for their own success; however, the recommendations apply to all students involved in experiential placements. I have observed that students who exhibit certain behaviours and avoid other behaviours achieve a higher level of success and view their experiential training as being more rewarding and fulfilling. In short, the top performers consistently provide patient-centred care and perform to the best of their ability with a high level of professionalism. My hope is that students who are open to considering the behaviours and attitudes described in this article will find their clinical placements more successful overall.
Some of the strategies may already be known, or may be considered intuitive, common sense or possibly too obvious to even mention. Thus, for many, these strategies will simply serve as a review. Nevertheless, due to the range of extant pre-placement experience, personality types, motivation and self-directedness, some students may have more or less self-discovery to do to ensure their success in an experiential placement.
Preceptors are invested in the student’s performance. The preceptor’s responsibility is to facilitate the development of knowledge, clinical skills and professional attitudes characteristic of their profession through guidance, coaching, role modeling and personal development of the student. The preceptor also helps to orient and socialize the student to the clinical environment to optimize learning.
The success strategies reflect my own views and are subdivided into two categories, the obvious and the not-so-obvious, but this is arbitrary and used primarily to pique the reader’s interest, since no strategy is more important than another and a student may find the most valuable strategy in either of the columns in Table 1.
The obvious strategies reflect what I perceive to be expected student behaviours and I believe they are reliably demonstrated by most students. I mention them primarily for the benefit of those few students who lack self-awareness or who fail to approach the experiential placement with the necessary significance. Nonetheless, making these strategies explicit will serve as a review for the majority.
The not-so-obvious strategies reflect what I consider to be anticipated student behaviours based on their preparation from school but may not be demonstrated universally. Students who do not demonstrate these strategies may be simply unaware of them or they may represent areas for growth. Regardless, these strategies will likely be particularly helpful for students who fit any of the following descriptions: have little clinical experience, are reluctant to participate in care for whatever reason, have difficulty picking up on environmental cues, fail to see the applicability of their current clinical placement to future practice, are unaware that their behaviour is being monitored by everyone on the team, or who fail to appreciate the expertise of their preceptor. Making these strategies explicit may be a revelation for those students.
The obvious strategies
- Understand and fully appreciate the syllabus provided by the educational institution to guide students in clinical placements. The clinical placement syllabus will help you take charge of your learning and along with pre-placement preparation will ensure that you meet rotation goals and requirements. The syllabus is intended to foster directed self-learning and independence, so that the student is not completely reliant on the preceptor for their learning. This enables the preceptor to guide the learner in their self-directed pursuit of real-world experiences.
- Appear interested at all times and show that you value this experiential opportunity. Show up for work well rested, alert and attentive to learn. Take responsibility for your behaviour to demonstrate independence and maturity, which are necessary traits for any workplace.
- Show enthusiasm for learning. Take initiative in addressing your learning objectives and demonstrate self-directedness, but ask for direction if needed. Demonstrate your ability to carry your learning forward to the next day.
- Demonstrate independence. Students who take charge of their learning and demonstrate independence are progressing toward the goal of becoming a competent practitioner. Some of the ways in which students demonstrate independence include taking initiative, initiating contact with patients and the healthcare team, taking responsibility for monitoring outcomes of therapy, advocating on the patient’s behalf, substantiating their recommendations with evidence, and handing off care to the next responsible person when appropriate. By the second week of the placement students should be aware of routines, work flow and expectations, and be able to set their own agenda to accomplish their identified learning needs.
- Show initiative and make contributions in the clinical setting. Experiential placements are a wonderful opportunity to engage in the various aspects of patient-centred care. Students should be motivated to provide care and contribute to their full scope of practice. Students who show initiative and are open to new experiences have a more rewarding rotation, a bigger impact on patients and the team, and receive more praise. Similarly, students who get involved in various rotation activities fit in faster, acquire more skills, pick up clinical pearls more easily and feel more confident. Students are encouraged to look for opportunities to be involved in care, since too much observation can slow the pace of skill development and maturation.
- Share your knowledge to gain new insights. You are expected to demonstrate your knowledge but are not expected to know everything. An experiential placement is an opportunity to consolidate your knowledge by applying what you know to real life situations, to gain new or greater insights into the application of the therapeutic thought process, and to gain new knowledge and skills through exploration and exposure to patients and practicing clinicians. Your preceptor will help you realize the potential of your fund of knowledge and encourage new learning. Identifying learning gaps through discussion with the preceptor will help you focus your learning.
- Be ready to discuss patient care issues with your preceptor. Use your available time to achieve your learning objectives and be prepared for discussions with your preceptor or the team. Read assigned material, complete patient work-ups in a timely manner and obtain the perspective of other team members as appropriate in advance of discussions.
- Be inquisitive, but expect to answer (most of) your own questions. Inquisitiveness demonstrates curiosity for learning, allows you to express your therapeutic thought process, drives productivity and personal development, and reflects engagement and independence. However, be mindful that inquisitiveness is only virtuous to the extent that it inspires self-directed learning and fosters self-discovery.
- Do not fall behind with your assignments. Establish expectations with the preceptor on day one of the rotation. Fulfilling rotation expectations according to the recommended schedule is important because it enables formative feedback.
- When responding to your preceptor or another care provider, never make anything up! Offering a vague or inaccurate generalization to a clinical question is not useful and may be construed as trivializing the situation. At worst, your response may be put into action and result in patient harm. However, it is perfectly acceptable to engage in a discussion with your preceptor regarding material that you are unsure of to identify the learning needs.
The not-so-obvious strategies
- Use clinical reasoning as the basis for your contributions to care. Clinical reasoning involves the amalgamation of inputs such as core knowledge and cognitive processing using your profession’s model of care. It requires the analysis and synthesis of information and knowledge and reflects your understanding and will be the basis of your expertise. The clinical reasoning skills you acquire will enable you to solve future clinical problems. Expertise is more than just looking up information.
- Integrate yourself into the placement environment to optimize learning. Integrating yourself into the learning environment enables personal growth. Despite the preceptor’s efforts, some students do not integrate quickly into their new team. Students who are reserved, reticent, quiet, shy or feel intimidated by the environment need to put these personal feelings aside so that academic performance is not compromised. Students need to feel they are welcomed by the preceptor and the clinical team, that their work is valued and that their presence enriches the learning environment. If you are slow to fit in, the surest remedy to employ is to simply do your best work.
- Discuss your observations with your preceptor. Reflect on your learning or on an interaction you have had at the site to gain further appreciation for the significance of events. Reflection and debriefing are powerful learning tools. The power of the clinical experience is magnified when issues are discussed or pointed out.
- Receive questions from other team members with grace and appreciation. Treatment-related questions directed to you by another healthcare professional represent an invitation into the patient’s circle of care, which is an honour. Your response to these questions is part of your contribution to patient care and teamwork, and reflects positively on you, your profession and your educational institution. Always clarify the timeline for your response, since the urgency for providing a response will vary with each clinical scenario.
- Consider therapeutic recommendations carefully because they will likely be put into action. Constructive working relationships among healthcare professionals are built on trust and respect. Such environments foster the student’s development of clinical skills. You should be aware that the healthcare team will assume your treatment recommendations are accurate and have been endorsed by your preceptor and therefore, they will likely be accepted and enacted. Remember, the team will expect you to emulate the diligence and professionalism exhibited by your preceptor.
- Embrace spontaneous learning experiences. You must be “present” in routine clinical encounters to gain experience. Each interaction with a patient or physician or other healthcare professional is unique and has something to contribute to your development. Presence in the environment enables you to participate in care decisions and follow up on outcomes. You will be able to observe how other care providers apply their clinical skills, and interact with patients and colleagues—yielding valuable lessons in teamwork.
- Be respectful of the clinical environment. Be cautious when using electronic devices when in the presence of the team. Clarify the culture at the site regarding use of hand-held electronic devices or ask permission if unsure. Observe how others make use of hand-held electronic devices. It is also important to be aware of space and computer access limitations and make appropriate accommodation.
- Use the mentorship and coaching skills of your preceptor. The preceptor-student interaction is dynamic and no two preceptor-student relationships are identical. Preceptors have much to offer their students and students have much to gain. Mentorship and coaching are two important benefits that preceptors provide for their students. Mentors pose thoughtful questions to their students that enable the student to evaluate their options and formulate their own decisions. Coaches help their students to refine their skills, experience new things, learn in new ways, expand their capacity, think creatively and grow in confidence. This process sometimes takes a student out of his or her comfort zone, however the resulting growth is rewarding and fulfilling. Receive feedback graciously and respond appropriately.
- Be appreciative of the time and energy being invested in you by your preceptor or other clinicians. All professions and trades devote considerable effort to grooming the next generation of practitioners. Students should think carefully about their learning objectives for each rotation and be sure they accomplish those objectives while the responsibility is shared with a mentor. Acknowledging the time invested by others in your development by expressing thanks demonstrates maturity and promotes further investment. For example, when appropriate say: “Thank you” (two of the most important words in any language), “I enjoyed that discussion”, “I found that discussion helpful”, and “Thank you for demonstrating that skill”, “That’s good feedback”.
- Consider your experiential placement as an extended job interview. While the student is focused on completing academic requirements, work colleagues are evaluating the student’s attitude, behaviour and work quality. Ensure that your conduct will enable the preceptor to consider you for employment or provide a good reference. Be sure to demonstrate your flexibility to accommodate various situations that arise in the work place. Offer suggestions to overcome challenges and demonstrate your ability to accept responsibility. The relationships you develop during the placement will be helpful to you in your career.
Conclusion
The strategies presented here can be valuable to students and preceptors as guidance for ensuring student success in experiential placements. While this list of strategies is neither comprehensive nor a formula for success, awareness of these behaviours can help students perform to the best of their ability. I believe there is value in making certain behaviours explicit for new learners.
I have avoided making comments about personality because I do not believe it should be the prominent driver of performance in a placement. Each student has their own skill sets, talents and personality and expresses himself/herself in their own way and to the best of their ability, and this makes each one unique. Attempting to change aspects of someone’s personality to affect his or her performance in a placement leads to frustration for all parties and can be a source of conflict.
Hopefully students and preceptors find at least one strategy here that helps the student achieve their learning objectives, facilitates their socialization to the team and leads to a successful experiential placement.
Human Airway Branch Variation and Chronic Obstructive Pulmonary Disease
Submitted by: Kayla Kok
Fanshawe student Kayla Kok reviews and summarizes a published article on a previously unknown genetically-inherited risk factor for COPD. The full article can be found at DOI: 10.1073/pnas.1715564115
Introduction
Despite being the globe’s third leading killer, the risk factors for Chronic Obstructive Pulmonary Disease (COPD) have long been a mystery. Aside from the genetic disorder alpha 1-antitrypsin deficiency, it has never fully been understood why some non-smokers develop diseases such as COPD, and yet lifelong smokers may not.
Thanks to the work of researchers in the study Human airway branch variation and chronic obstructive pulmonary disease[i], lead by Benjamin Smith, some light has been shed on this very topic. These researchers have discovered a previously unknown genetically-inherited risk factor for COPD. Their work has revealed that central airway branching variants can increase one’s risk of developing COPD and other respiratory illnesses and that an incredible 26.5% of the world’s population has one of these branching variants.
The Methodology
Smith and team examined Computed Tomography (CT) scans of 3,169 people in the Multi-Ethnic Study of Atherosclerosis (MESA) Lung Study[ii]. The mean age was 69, and 48% were male. The ethnic distribution among the participants was 39% Caucasian, 27% African-American, 21% Hispanic and 13% Asian-American. Fifty four percent were current or former smokers with a median exposure of 15 pack years.
Researchers also combined the data from MESA with results from the Subpopulations and Intermediate Outcome Measures in COPD Study, or SPIROMICS, to gather data from a pool of 3,363 participants, 1,212 of whom had been diagnosed with COPD.
Among the participants, airway branch variations were present in 26.5%, while 73.5% had standard airway anatomy (figure A). The most common variant (figure B) was seen in 16% of participants, and consisted of an accessory subsuperior airway. This variation was more common among Caucasians, and less common among Asian-Americans. The second most common, seen in 6%, was an absence of the right-medial basal airway (figure C). This variation was more common in Asian-Americans, and less among African-Americans. The remaining 4% of participants had rare branching variants.

Findings
When researchers compared the results of those with regular airway anatomy to those with branching variations, participants with variations were shown to have a higher risk of developing COPD.
When compared to those with normal airway anatomy, those with an accessory subsuperior airway had a 40% greater chance of developing COPD, regardless of whether or not they were smokers. Participants with an absent right-medial basal airway had a 55% greater chance of developing COPD if they were non-smokers, a risk that increased to 78% for smokers.
However, it was not just branching patterning that varied among participants. Both variations were found to have predictable changes throughout the entire lung, which researchers believe further contribute to the increased risk of disease development.
The most common branching variation, the accessory subsuperior airway, was found to have segment lengths that were 3.7% shorter than average throughout the entire lung, not just in the accessory lobe. The presence of an accessory subsuperior airway also demonstrated larger airspace in all lobes, and a higher number of central airway bifurcations.
While the variant which causes the absence of the right-medial basal airway was found to have segment lengths statistically similar to normal airway anatomy, the airway lumen throughout the lungs was found to be significantly narrower.
Associations between these branch variants and the likelihood of developing COPD did not differ by gender, race, ethnicity, presence of childhood asthma, second-hand smoke exposure, or maternal smoking during pregnancy.
Heritability
Because of the central positioning of these common variations, researchers hypothesized that their absence or presence did not change in adulthood. They compared CT scans from 300 MESA participants spanning a ten year interval, and there were no significant changes. This suggested to researchers that the branch variations did not occur in adulthood.
As the variants were found to be stable, researchers further hypothesized that these variations were indeed heritable. They selected 16 unrelated MESA participants with variant anatomy and conducted a CT scan on the participants’ siblings.
Among siblings, the presence of an accessory subsuperior airway was 46%; higher than the 16% prevalence among the general population. The absent right medial-basal airway was prevalent at a rate of 31% among siblings, also greater than the prevalence of 6% among the general population. Given these findings, the researchers further hypothesized these variations reflected differing function of the genes which regulate airway morphology.
Researchers conducted a targeted gene analysis of 109 single nucleotide polymorphisms (SNP) located on 11 genes. Two SNPs on chromosome 5 were associated with the absence of a right medial-basal airway. None of the selected SNPS were found to be associated with the presence of an accessory subsuperior airway.
Discussion
One’s central airway is essential for the removal of harmful particulate matter. Anything that impedes the removal of inhaled debris may lead to an increased likelihood of disease development and interstitial damage. Prior to the conduction of this study, it was unlikely many people would have thought of the anatomy of the central airways when considering risk factors for pulmonary diseases.
Smith and team believe that the increase in COPD risk among these lung variations is not due to the branching pattern themselves, but because of the associated changes that were found to accompany them. The increase in the amount of central airway bifurcations in the accessory subsuperior airway creates an increase in area for sedimentation of particulate matter. The narrower airway lumen associated with the absence of the right-medial basal airway greatly affects airway resistance. All of these changes lead to a decreased ability to clear harmful matter from one’s lungs.
These findings suggest that airway branch variations, which are common and easily identifiable, reflect widely altered lung structure and provide a genetically determined basis for COPD susceptibility, even among those who do not smoke. Smith and team are hopeful that in the future preventative and therapeutic interventions, based on the presence of abnormal lung morphologies, may one day improve patient outcomes.
Though the best way to prevent one’s chances of developing COPD is still to abstain from or quit smoking, perhaps one day in the future healthcare practitioners will be able to warn patients that this risk factor for COPD runs in their family, and to choose their habits accordingly.
[i] Smith BM et al. Human airway branch variation and chronic obstructive pulmonary disease. Proceedings of the National Academy of Sciences of the United States of America E (2018): 974-981.
[ii] Smith BM, et al. The Multi-Ethnic Study of Atherosclerosis (MESA) COPD Study and the Subpopulations and Intermediate Outcomes in COPD Study (SPIROMICS) Comparison of spatially matched airways reveals thinner airway walls in COPD. Thorax. 2014;69:987–996. [PMC free article] [PubMed]
EYE ON
Unique Funding Model for Pulmonary Rehabilitation in North Bay and Vaughn, Ontario
Tammy Draper looks at a unique funding model for pulmonary rehabilitation.
Submitted by: by Tammy Drape, RRT
British Lung Foundation (England and Wales). VAT 648 8121 18
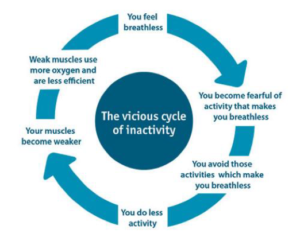
Having been an RRT for over 20 years, far too often I’ve seen patients discharged from hospital on oxygen, only to become socially isolated, less active or even sedentary, progressing to even more shortness of breath…and ultimately fall into the vicious cycle that often occurs with lung disease. They often feel like they’re alone.
 For every client that goes home on oxygen with CPR, we provide breathing techniques, strategies for coping with shortness of breath, and disease specific information. We also express the importance of staying active and understanding the downward spiral that they can easily fall into. Even further, we assess each of our clients to see if they may be good candidates for our “Community Pulmonary Rehabilitation program” or our “In Home Pulmonary Rehabilitation program.” By providing even the basics, we are able to influence the vicious cycle.
For every client that goes home on oxygen with CPR, we provide breathing techniques, strategies for coping with shortness of breath, and disease specific information. We also express the importance of staying active and understanding the downward spiral that they can easily fall into. Even further, we assess each of our clients to see if they may be good candidates for our “Community Pulmonary Rehabilitation program” or our “In Home Pulmonary Rehabilitation program.” By providing even the basics, we are able to influence the vicious cycle.
Who are we?
Centre for Pulmonary Rehabilitation (CPR) was established June of 2005 by Tammy Draper (Registered Respiratory Therapist) with over 20 year experience in pulmonary rehabilitation. CPR is unique in providing pulmonary rehabilitation and follows American Association of Cardiovascular Pulmonary Rehab Guidelines. Initially launched as a pulmonary rehab only, we soon realized patients who needed pulmonary rehab the most couldn’t afford it as the cost is approx. $2,200 per patient to run rehab for eight weeks, including all assessments and educational material. In an attempt to help decrease the cost of the pulmonary rehab, we accessed the “Prism” Program funded by Glaxo Smith Kline and Pfizer, however, this was only for a two year period. We had to come up with a solution so that we could reach all patients in need.
CPR’s business model is unique in the health care industry. CPR’s goal has been to “invest back into our community” by providing FREE pulmonary rehabilitation to those in need, while following best practices. Our solution: we became a Home Oxygen Vendor and a CPAP vendor. We reinvest proceeds from other revenue streams (home oxygen and CPAP/sleep therapy) into the pulmonary rehabilitation program, making it free. For the past nine years, pulmonary rehab has been free for all clients in need. Our business model has enabled us to help more patients in our community and provide the highest level of care possible. Without the support of home oxygen and CPAP referrals, we would not be able to provide this service.
A recent survey was conducted (Pulmonary Rehabilitation in Ontario: A Cross-Sectional Survey, March 2015 Ontario Health Technology Assessment Series; Vol. 15: No. 8, pp. 1–67, March 2015)
- The survey showed that the province has relatively few program spaces compared to the number of people who could use them.
- More than 700,000 people in Ontario have chronic lung disease.
- The facilities currently available in this province can support only about 1.12% of the people who could potentially benefit from pulmonary rehabilitation.
The Pulmonary Rehab Program includes: individual exercise assessment for improved endurance, improve strength to do daily activities, education on use of medications, disease specific patient and family education, active physician monitoring and intervention, breathing retaining, physical support, promote independence, smoking cessation counseling and motivation to continue maintenance.
Program Goals: Improve quality of life, reduce respiratory symptoms and exacerbations, increase knowledge of lung disorders, return to work or leisure activities, improve performance of aids to daily living and become an expert in their own care.
Quality Control (Measures Key Performance Indicators (KPIs): CPR has rigorous KPIs that are recorded and reported in a summary to each referring physician when a client graduates from our pulmonary rehabilitation program. KPIs include; six minute walk test, St. Georges Quality of Life Questionnaire and customer satisfaction survey.
What are the “best practices”?
Best Practices for treatment of COPD
- Quality Based Procedures: COPD

Quality-Based Procedures: Clinical Handbook for Chronic Obstructive Pulmonary Disease, Health Quality Ontario & Ministry of Health and Long-Term Care, January 2013,
- Canadian Thoracic Society: COPD
Actual Recommended


TOOL BOX

Be Open to Alternate Forms of Exercise for your Patients
Submitted by: Jane Lindsay, BScPT, CRE
When educators are encouraging patients to attend pulmonary rehabilitation, it is essential that they carefully evaluate each patient’s needs and preferences. A recent study, published online in Chest, was reviewed by the American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR). The study is a randomly controlled comparison of “standard” pulmonary rehabilitation (PR) and Tai Chi. Both groups of COPD patients were naive to rehabilitation, and attended sessions for 12 weeks: three times per week for the PR group, and five times per week for the Tai Chi group. While some limitations exist, as in almost every study, the short version of the result is that both groups demonstrated very similar improvements in exercise tolerance and in quality of life.
In Ontario, PR Programs are still regrettably few and far between, often with prohibitively long waiting lists. As stated by the AACVPR reviewer “As PR professionals, it is imperative that we are vigilant for innovations arising from published evidence regarding alternatives for PR components. While Tai Chi may be a reasonable alternative for typical PR exercise, consideration of PR professional expertise and patient preferences must be included in programmatic decisions.”
In my own experience, a ‘pre-rehab’ visit for patients on the wait list, during which patients were given guidance for their own exercise prior to attending the formal program, sometimes resulted in patients no longer feeling they needed formal PR since they had improved their function so much with home or community based exercise. Whether patients are on a waiting list, or do not have access to a PR Program, or just don’t see PR as a good fit, educators can feel confident recommending alternative forms of exercise and activity to most COPD patients who would also be appropriate for a PR Program.
To see the full AACVPR review of the study, go to:
http://newsandviews.aacvpr.org/blogs/emma-frey/2018/05/11/tai-chi-comparison-to-pulmonary-rehabilitation
To see the full article, use this doi:
https://doi.org/10.1016/j.chest.2018.01.053

IN THE SPOTLIGHT
Therese Hawn, BScPT
Throughout her career, Therese has contributed to the mission of the ORCS by furthering excellence in respiratory care through education, research, collaboration and professional expertise.
Submitted by: Lisa Wickerson, BScPT, MSc, PhD (Candidate)
hroughout her career, Therese has contributed to the mission of the ORCS by furthering excellence in respiratory care through education, research and interprofessional collaborations. Therese is a physiotherapist and an American College of Sports Medicine exercise specialist within the Peter Munk Cardiac Program at the University Health Network (UHN) in Toronto and the clinical physical therapy practice leader for cardiac, transplant, advanced medicine and surgery, and surgical oncology programs.
In her clinical and leadership roles at UHN over the past four decades, Therese has been instrumental in developing referral criteria and prioritization guidelines for physiotherapy weekend service, preparing the organization to achieve Accreditation with Exemplary Standing, and developing professional-level continuing education courses in cardiorespiratory physical therapy assessment, treatment and early mobility skills in acute and critical care. These courses have been offered on-site at UHN and tailored and delivered at a number of Ontario acute care, community and rehabilitation hospitals. She has fostered innovation in clinical practice at UHN by establishing different physical therapy coverage models in the cardiac program, promoting patient education through a site on the organization’s intranet and implementing the delivery of acupuncture in the intensive care unit, transplant and cardiac programs. She is a trained facilitator for interprofessional education (IPE), and has been involved in the UHN pain committee, and has actively contributed to the University of Toronto’s Pain Education Week. Therese is an American Physiotherapy Association credentialed clinical instructor who has mentored numerous physiotherapy students in the care of complex cardiac patients during clinical internships, and has been a role model and mentor for junior staff. Notably, she received the Wightman-Berris Academy Teaching Award for extraordinary contribution to education at UHN.
Therese is a long-time member of and contributor to the Ontario Respiratory Care Society, specifically in her role on the Editorial Board overseeing the preparation and publication content related to patient education and acute care. She has collaborated with UHN colleagues and academic faculty at the University of Toronto on different clinical research studies. Some of these collaborations include: evaluation of the two-minute walk test as a measure of functional capacity in cardiac surgery patients; characterization of weekend physiotherapy services in three tertiary hospitals in the greater Toronto area; the study of satisfaction and barriers to a class on physical activity for cardiac surgery inpatients; evaluation of physiotherapy treatment algorithms for cardiac surgery patients; examination of the role of a cardiovascular physiotherapist as a consultant; and the development of an inter-professional pre-operative assessment tool for cardiac surgery patients. This knowledge has been disseminated at scientific conferences as poster or oral presentations and published in peer-reviewed journals.
Best wishes in your retirement next year Therese!
RESPIRATORY ARTICLES OF INTEREST
Respiratory article of interest
Study one
Castro M, Corren J, Pavord ID, Maspero J, Wenzel S, Rabe KF, et al. Dupilumab Efficacy and Safety in Moderate-to-Severe Uncontrolled Asthma. The New England journal of medicine. 2018;378(26):2486-96.
Study two
Rabe KF, Nair P, Brusselle G, Maspero JF, Castro M, Sher L, et al. Efficacy and Safety of Dupilumab in Glucocorticoid-Dependent Severe Asthma. The New England journal of medicine. 2018;378(26):2475-85.
Submitted by: Elizabeth Gartner, BScOT
A review of the following two studies involving dupilumab efficacy and safety in patients with asthma:
Study one (S1) and study two (S2) both looked at the efficacy and safety of dupilumab in patients with asthma. Both studies used similar methods and patient populations, although S2 specifically investigated patients with severe asthma who were glucocorticoid-dependent. Both study patient populations consisted of those over 12 years old who had had a diagnosis of asthma, as defined by the Global Initiative for Asthma 2014 guidelines, for one year or longer.
Eligibility criteria in S1 included asthmatic patients receiving medium-to-high dose inhaled glucocorticoid and whose forced expiratory volume in one second (FEV1) before bronchodilator use was 80% or less of predicted normal (adjusted to 90% or less for ages 12-17) and reversibility of 12%. They also had a score of 1.5 or greater on the 5-item Asthma Control Questionnaire (ACQ-5) and worsening of asthma over the previous year. S2 patients differed in that those treated with systemic glucocorticoids in the last six months were eligible. Also, in the four weeks prior to the study their treatment included high-dose inhaled glucocorticoid. Both studies recruited patients with no minimum baseline blood or sputum eosinophil count.
Drug trial design was different in the two studies for randomization and intervention duration. Study 1 ran from May 2015 to September 2016, and involved 1902 patients assigned in a 2:2:1:1 ratio to receive either a 200mg or 300mg dose of dupilumab or the matched volume of placebo, every two weeks over 52 weeks. Study 2 ran from December 2015 to September 2017, and involved 210 patients who were randomized into two groups, either receiving 300mg dose of dupilumab or placebo. Treatments in S2 were also provided every two weeks, but for 24 weeks, and with glucocorticoid doses being adjusted from week 4 to week 20.
Results for both studies demonstrated positive outcomes using dupilumab in similar end points. Primary end points in S1 included severe exacerbations per year and FEV1 absolute change from baseline, before bronchodilator use. Primary efficacy end point for S2 was percentage reduction in glucocorticoid dose, from baseline to end of study with asthma controlled. Other efficacy end points were the same as in S1.
Scores in the ACQ-5 for S1 from two weeks in, until the end of the study showed improvement in asthma control with dupilumab over placebo. The S2 ACQ-5 scores reported at the end also showed improvement in asthma control with dupilumab over placebo. Incident rates of adverse events were similar in both treatment and placebo groups across the studies.
In conclusion, both of these studies indicated that the use of dupilumab in patients with moderate-to-severe asthma as well as in those patients with glucocorticoid-dependent severe asthma, reduced rates of exacerbation, increased FEV1 and improved asthma control.
Respiratory article of interest
Jolly K, Sidhu MS, Hewitt CA, Coventry PA, Daley A, Jordan R, et al. Self management of patients with mild COPD in primary care: randomised controlled trial. BMJ (Clinical research ed). 2018;361:k2241.
Submitted by Julie Duff Cloutier RN, MSc
The study was designed to evaluate the effectiveness of telephone health coaching to support self-management delivered by a nurse in a primary care population with mild symptoms of chronic obstructive pulmonary disease. A multicentre randomised controlled trial was conducted which involved 71 general practices in four areas of England. The 577 patients with a Medical Research Council dyspnea scale score of 1 or 2, were randomised to telephone health coaching (n=289) or usual care (n=288). The intervention consisted of telehealth coaching aimed at supporting self-management in relation to smoking cessation, physical activity, inhaler technique and medication adherence, and was delivered by a nurse, while the usual care group received a standard information leaflet on self-management. The primary outcome was health related quality of life measured at 12 months. Secondary outcomes included dyspnea, self-reported physical activity and psychological morbidity amongst others. No significant differences were noted between the intervention and usual care groups, however, this study is one of few conducted with those who have mild disease. Further research targeted towards this patient group is needed.
WAYS TO GET INVOLVED
Ontario Respiratory Care Society (ORCS) Committees
Joining an ORCS Committee is a great way to get involved!
Provincial Committee
The Provincial Committee provides leadership to the ORCS and is comprised of the ORCS Chair, a Chair-Elect or Past Chair in alternate years, the Chairs of the five standing committees, the Chairs of the regional planning committees and a member of the Lung Health Foundation Board of Directors.
Editorial Board
Produce an electronic publication for the Ontario Respiratory Care Society (ORCS) members; provide academic content for the publication.
Respiratory Health Educators Interest Group (RHEIG)
Provide respiratory education and a half-day session at the Better Breathing Conference; provide patient education content for the ORCS publication.
Membership Engagement Committee
Recruit and build membership for the Society.
Education Committee
Session planning for the Better Breathing Conference.
Research and Fellowship Committee
Manage the funding process including Grant and Fellowship application review and funding allocation.
Regional Planning Committees
Regional Planning Committees plan educational events in their respective regions. The Regions include:
Northeastern Region
Northwestern Region
Eastern Region
Central Region
Western Region
To find out more, or to join one of these Committees, contact the OTS/ORCS Coordinator,
Natalie Bennett, nbennett@lungontario.ca
EDITORIAL Committee
CO-CHAIRS
Jocelyn Carr, BScPT, MSc
Lorelei Samis, BScPT
MEMBERS
Julie Duff Cloutier, RN, MSc, CAE
Yvonne Drasovean, RRT
Elizabeth Gartner, BScOT
Lawrence Jackson, BScPhm
Rachel McLay, HBSc (Kinesiology)
Shirley Quach, HBsc, RRT
Priscila Robles, BScPT, MSc, PhD
Lily Spanjevic, RN, BScN, MN, GNC(C), CRN(C),CMSN(C)
RHEIG Executive Team
CO-CHAIRS
Jane Lindsay, BScPT, CRE
Lorelei Samis, BScPT
MEMBERS
Michael Callihoo, RRT, CRE
Rose-Marie Dolinar, RN(EC), MScN, PhD student
Diane Feldman, RRT, CRE
Olivia Ng, BScPhm, RPh, PharmD (Candidate)
Kitty Seager, CRE, CTE, RPN
Maria Willms, RN, CRE
CHAIR, ONTARIO RESPIRATORY CARE SOCIETY
Dina Brooks, BScPT, MSc, PhD
PRESIDENT & CEO, THE LUNG HEALTH FOUNDATION
George Habib, BA, BEd, CAE
DIRECTOR, ONTARIO RESPIRATORY CARE SOCIETY
Sherry Zarins
OTS/ORCS Coordinator
Natalie Bennett