An official publication of the Ontario Respiratory Care Society, a section of The Lung Association – Ontario.
Update Ontario Respiratory Care Society
Update on Respiratory Health, Research and Education is a publication of the Ontario Respiratory Care Society, a section of the Lung Association. Update is published three times per year and includes peer-reviewed original articles, clinical practice tools, health news, and communications between the ORCS and its membership.

CHAIR’S MESSAGE
Happy New Year!! 2017 has been a year of growth and progress for The Lung Association – Ontario and the Ontario Respiratory Care Society. We are excited about the new ORCS member portal that launched in the fall. The new portal is a streamlined system that puts membership management, communications and events all in the one place. The new portal greatly improves the ORCS registration process for returning and new members, allows members to have their own profile page, and streamlines Better Breathing and other event registrations. If you haven’t done so already, visit https://lungontario.ca/for-health-professionals/ontario-respiratory-care-society/ to create or update your profile today!
Better Breathing 2018, Jan 25 – 27, is almost upon us. Canada’s premier respiratory conference caters to a variety of health-care disciplines including respiratory therapists, nurses, physiotherapists, pulmonary function technologists, occupational therapists, social workers, pharmacists, dietitians, and others involved in various aspects of respiratory care. This year’s line-up includes sessions on Transplant Innovations, the Use of Apps and New Technology in Sleep Medicine, Compassion Fatigue for Health-care Workers, and a lively (if I may say so myself) debate on pulmonary rehabilitation versus general rehabilitation when treating COPD. New this year will be a Respiratory Therapy Society of Ontario (RTSO) education stream featuring acute and community sessions, as well as the RTSO sponsored poster session and cocktail reception. For more information please see the Better Breathing website, https://lungontario.ca/for-health-professionals/better-breathing-conference.
And finally, The Breathe! Gala returns on Thursday, January 25, 2018 at the Liberty Grand – one of Toronto’s most prestigious venues. Tickets are discounted for Better Breathing delegates. Purchase tickets here. I hope you can join us for an evening of celebration and help us continue to create breathing breakthroughs!
I am always available to discuss any comments or suggestions that you may have. Feel free to contact me by email dina.brooks@utoronto.ca or by phone 4l6-978-1739. I’m looking forward to seeing you at Better Breathing 2018!
Respectfully submitted,
Dina Brooks, BScPT, MSc, PhD
Chair, Ontario Respiratory Care Society

EDITOR’S MESSAGE
Welcome to the Winter 2018 edition of Update on Respiratory Health, Research and Education. The Editorial Board and Respiratory Health Educators Interest Group (RHEIG) continue to work hard to bring you interesting and informative articles in this joint ORCS/RHEIG publication and we hope these will enhance your knowledge about various areas of lung health.
Our first feature article Protection of Lung Health of Poultry Farmers in Ontario: Results of Outreach Rural Lung Health Clinics with N95 Respirator Fit-testing, has been written for us by Rose-Marie Dolinar while the second feature article by Donna Pan is titled Youth as Social Change Makers.
While our In the Toolbox section provides a review of Common Asthma Triggers: An Education Companion, which was developed for use with people with low literacy or English as a second language, our Eye On section presents the after-school program Play for All which promotes lung health and activity in children in primary school. In our Respiratory Articles of Interest section we provide summaries of two articles: one relates to asthma in athletes, and the other to painful co-morbidities in those with COPD. Lastly, but in no way least, In the Spotlight shines the light on our talented Shelley Provost.
As you know Better Breathing 2018 is only a number of weeks away and we encourage you to attend this excellent conference along with the Thursday afternoon sessions just prior to the conference, which are sponsored by the RHEIG. Please check the website and set aside January 25 to 27, 2018 so that you can join us in Toronto at Better Breathing 2018.
As we provide you with this joint electronic publication, we look forward to hearing from you with feedback, so, please, do let us know what you think!
Respectfully submitted,
Jocelyn Carr, BScPT, MSc
Co-chair Editorial Board

The Lung Association – Ontario Board Member, Donna Cansfield, MPP Kathryn McGarry, MPP Ted McMeekin, MPP France Gélinas and The Lung Association – Ontario President and CEO, George Habib at Queens Park to celebrate the establishment of The Ontario Lung Health Consultation Group.
The Ontario Lung Health Act
Lung disease affects millions of Ontarians – not just the 2.4 million people who live with a chronic respiratory illness, but also the millions more who love and care for them. For the past 10 years, The Lung Association and its partners have been calling on the Government of Ontario to establish a Lung Health Action Plan in order to properly and effectively address lung disease in the province. Of the four chronic diseases responsible for 79 per cent of deaths (cancers, cardiovascular diseases, lung disease and diabetes) lung disease has been the only one without a dedicated province-wide strategy – until now.
Inspired by what this action plan represents, the three political parties of the Ontario Legislature came together in a demonstration of true non-partisanship and commitment to the health of Ontarians, and reached an agreement to pass Bill 71, Lung Health Act, in the final days of the fall 2017 legislative session.
On Tuesday, December 12th in the Ontario Legislature, Bill 71 was passed by unanimous consent, and on Thursday, December 14th the Bill received Royal Assent from the Lieutenant Governor, officially enacting into law The Ontario Lung Health Advisory Council.
This group will be dedicated to providing provincially-based advice and recommendations on lung health to the Minister of Health and Long-Term Care to make improvements in lung health awareness, diagnosis, treatment and care. Its goal will be to work towards the development and implementation of an Ontario Lung Health Action Plan that will provide a coordinated approach to prevent lung disease, improve patient outcomes and reduce healthcare spending.
Your Lungs, Your Life, a report produced by The Lung Association, estimated that lung disease cost taxpayers approximately $4 billion in 2011. By 2015 that estimate grew to more than $27 billion in direct and indirect healthcare costs. Perhaps what is most troubling is that that cost is expected to balloon to more than $76 billion by 2021, which represents an astonishing estimated 1800 per cent increase in cost over a 10 year period.
While the Lung Health Act itself is now confirmed, much work still remains. Over the coming months, we will continue to work closely with the Ministry of Health and Long-Term Care on the development of the Advisory Council and its structure, and look forward to sharing more information with you as it becomes available.
Our collective breathing future has just became much brighter. Thank you to the members of the Lung Health Caucus, members of our professional societies, our donors, partners, volunteers and staff for all of your support in getting us to where we are today. With you by our side, we are helping even more Ontarians breathe.
Dr. Patricia Hill Bailey
On Wednesday November 15, 2017 (World COPD Day), the respiratory health community in Canada lost a true champion; her family lost a loving and caring mother, grandmother and sister and I lost a very special friend. It was on that day that Dr. Patricia Hill Bailey passed away from cancer at Health Sciences North in Sudbury. Pat was a wonderful, kind person with a great sense of humour and a strong commitment to nursing, research and education. She was one of the earliest leaders of the Ontario Respiratory Care Society (ORCS) which she joined in the 1980s. Her many volunteer contributions to the ORCS were extraordinary and continued even after her retirement as a faculty member in the School of Nursing at Laurentian University in 2014.
Over the years Pat served in numerous ORCS volunteer positions including regional representative for Northern Ontario, President-Elect, President (now called Chair), Past President and member of the Editorial Board, Research and Fellowship Committee, Education Committee and many regional seminar planning committees. Pat was committed to engaging in efforts that aimed to enhance the care of individuals living with chronic lung diseases and their families. She was also supportive of professional education initiatives for health-care professionals in the north.
Pat trained as a staff nurse in Winnipeg and later worked as an ER charge nurse in Toronto. She completed a BN at McGill University and a MHSc degree at McMaster University in Hamilton before joining the faculty of the School of Nursing at Laurentian University in Sudbury. She completed her PhD at the University of Edinburgh – one of her proudest accomplishments. Her particular area of expertise, for which she was recognized nationally and internationally, was qualitative research. She was passionate about the importance of health-care professionals seeing illness, especially acute exacerbations of COPD, from the perspectives of patients and their family caregivers, avoiding the stigma of smoking-related lung disease.
An expert in her field, she was widely published in professional publications and peer-reviewed journals and presented posters and lectures at local, provincial and national conferences. Pat made numerous contributions to the lives of so many students, colleagues, friends, patients and to the discipline of Nursing. She always encouraged her students to achieve their full potential, supporting their pursuit of Masters and PhD degrees and their involvement in professional organizations such as the ORCS and the RNAO. She also contributed her expertise to the RNAO’s Best Practice Guidelines for both COPD and asthma.
Pat was funny and fun to be with. She was very proud of her children and grandchildren and cared deeply for her family, colleagues, students and friends. She will be greatly missed and forever remembered.
Sheila Gordon-Dillane, ORCS Director 1990 – 2015
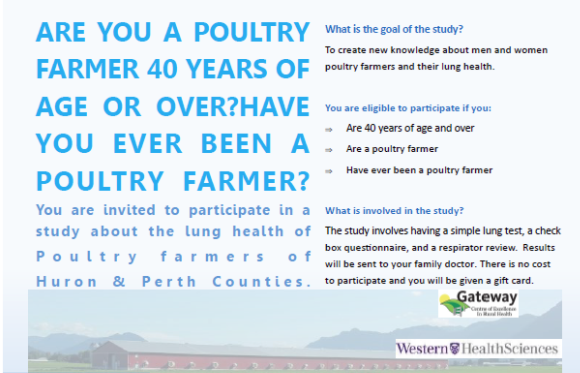
Protection of the Lung Health of Poultry Farmers in Ontario: Results of Outreach Rural Lung Health Clinics with N95 Respirator Fit-testing.
Rose-Marie Dolinar MScN, RN(EC), PhD(C), The University of Western Ontario
Introduction
Chronic obstructive pulmonary disease (COPD) is a leading cause of morbidity and mortality in Canada1. COPD develops slowly over time and Canadian farmers with COPD often present for health care in late stages of the disease because they accept cough or breathlessness as “normal”, and because access to health clinics, and the timing of appointments may be limiting factors. COPD is preventable and is easily detected2. Knowing lung health risks, and protecting the airways by wearing the appropriate fit-tested respirator, reduces exposure to harmful respiratory hazards.
Changes in agriculture affecting lung health
Agriculture in Canada has grown from single family farms, to large-scale farming operations in response to the shift of populations to large urban centres. In 2011, over 80% of Canadians lived in urban centres3 compared to over 80% being rural dwellers in Canada in the early 1900s.
Because of this population shift, farming operations such as poultry production have moved towards industrial large-scale confinement facilities. Dust particles in poultry barns can be comprised of bird feed, bedding material, bird feces, feathers, dander, and bioactive components of bacteria, fungi/molds, dust mites and endotoxins (cell wall components of gram-negative bacteria), all of which could trigger cellular reactions within the lung tissue4. Studies have identified that poultry workers’ exposure to bioactive dust affects the health of the lungs and is a potential occupational hazard5,6.
As the dust is inhaled, the particles can deposit along the conducting airways, as well as reach the respiratory units of the lungs. The smaller the dust particles, the deeper they can reach within the lungs.
Dust within a poultry barn can range in size, from large visible-to-the-eye dust particles (greater than 20 microns), to microscopic dust particles (less than 0.3 microns). To put this in perspective, the diameter of human hair is approximately 80 microns, and the diameter of the respiratory bronchioles is between 500 and 800 microns8.
Particles smaller than 10 microns in diameter have the potential of causing biologic harm to the lungs of susceptible individuals7,8. Over time, dust exposure can harm the respiratory units of the lungs, and start the progression of COPD. The good news is that COPD is a preventable and treatable condition2,10.
Protection of lung health
According to a Canadian study with non-smoking participants who have not previously been exposed to a swine barn environment, wearing of an N95 disposable respirator can significantly reduce acute lung health effects11. Respirators, when fit-tested to reduce air leaks, will perform better, and have a greater ability to protect lungs from biohazardous dust. There is greater danger in wearing a respirator that has air leaks, since the worker will assume that he or she is protected.
According to the Canadian Standards Association Z94.4-11 “Selection, use and care of respirators” (2016), workers should wear respiratory protection at all times in areas with atmospheric hazards and inspect the respirator prior to use; maintain and store respirators in accordance with training and manufacturer’s recommendations; perform seal checks after donning a respirator; be clean shaven when wearing respirator and understand the limitations associated with the use of respiratory protection12.
N95 is a designation of a respirator that has been approved by the National Institute of Occupational Safety and Health (NIOSH, 2014) to block at least 95% of very small (0.3 micron) airborne particles13.
Knowing the hazard within the poultry barn is essential to knowing which type of respirator to wear. Table 1 provides a summary of different types of respirators, matched to the lung health hazard.
Table 1: Lung health hazards within poultry barns and recommended type of respirator
| Hazards found in Poultry Barns | Type of Respirator | How the respirator protects from the hazard |
| Bioactive dust | N95 disposable respirator | Needs respirator fit-testing in order to protect. “N” means the respirator is not resistant to oil and is 95% efficient13. |
| Ammonia | Air-purifying, full-face-piece respirator (gas mask) with two canister providing protection specifically against ammonia | Needs respirator fit-testing in order to protect. The recommended level for short-term exposure (15 minutes) is no greater that 35 ppm. Many poultry producers become accustomed to the ammonia, and are less able to detect ammonia gas below 50 ppm14. |
| Carbon dioxide, hydrogen sulfide, carbon monoxide | Air-supplied respirator needed | Fit testing is not needed, since air is supplied within a hood over the head. |
Learning about the work of poultry farmers was essential for planning an effective lung health study. A series of meetings were held between the poultry farmers and the author, to plan for the outreach rural lung health clinics. The Poultry Producers Lung Health pilot study was launched, after obtaining ethics approval from the University of Western Ontario, Research Ethics Board.
Methods
The lung health clinics’ times and locations were decided in collaboration with the farmers, to fit between harvest times, and in close proximity to their farms. The lung health clinic appointment sections devoted to lung health protection included four steps:
Step 1: Each participant completed a lung health questionnaire, developed specifically by this author for the poultry producers, which contained specific lung protection questions, asking each poultry farmer:
- the number of years working in a dusty environment,
- to identify from a list, the lung health risks in the poultry barn,
- how often they wear their respirators,
- what information they would find useful in protecting their lungs.
Step 2: After the questionnaire was completed, a review of the lung health risks and respirators types for each lung health risk was discussed.
Step 3: The farmers participated in a standardized N95 respirator fit test. Each participant was given a choice of three N95 respirators, to try on, and see which they found most comfortable and fit best. Next, each participant tested their respirator for leaks during inhalation and exhalation to confirm a suitable seal, and were asked if they tasted or smelled a scent when the respirator was on, under a paper-like hood.
Step 4: After three months, a questionnaire was sent to each participant, to ask how often they wore their fit-tested respirator.
Results
Two rural lung health clinics were held in Seaforth, Ontario and Clinton, Ontario, on August 3 and August 4, 2016, respectively. Eight participants per day attended 1-hour long appointments, for a total of 16 poultry farmers (N=16). The average age of participants was 56.8 years (SD 9.74), with 82% males, and 18% females. Table 2 summarizes the results of dust exposure, occupational risks present in poultry barns, respirator use all of the time, and information and resources that would be useful to help protect their lungs.
Table 2: Results from the Lung Health Questionnaire
| Lung health question | Result (N=16) |
| Average exposure to farm dust in years | 38 yrs (SD 14.95) |
| Occupational risks identified | Organic dust 100% Ammonia 81.2 % |
| Wearing of respirator all of the time | Baseline 6.3% 3 months 18.8% |
| What information and resources would be useful to you in your job, to help you protect your lungs? | 25% requesting more information about respirators |
Respirator training and fit-testing of N95 respirators results:
- Each participant chose one of the three N95 respirators that fit best,
- Each participant demonstrated no air leaks (good seal) prior to N95 fit-test,
- Each participant performed safe donning (putting on) and doffing (taking off) of respirators after demonstration.
Conclusion
There is a need for more outreach lung health clinics and respirator training opportunities for farmers in Ontario, to address the urgent need for protection of lung health and the prevention of COPD. The present study demonstrated that rural lung health clinics are well-attended at 100% when location (close proximity to the farming community), and timing (between harvests) are planned in collaboration with the farmers through knowledge exchange.
The need for more respirator training has been identified by the farmers. Rural lung health clinics offer one way to deliver the training. Websites dedicated to lung health protection, with videos, may be another way to reach to the farmers who live across large geographic areas of Ontario, however N95 fit-testing would require face-to-face appointments. Respiratory care professionals are needed to deliver this training, in our efforts to prevent chronic lung disease and promote the lung health of farmers.
Funding for this study was provided by The Lung Association through an Ontario Respiratory Care Society Fellowship Award.
This study was supported by the Gateway Centre of Excellence in Rural Health.
References
1. OʼDonnell, D.E., Hernandez, P., Kaplan, A., Aaron, S., Bourbeau, J., Marciniuk, D., Balter, M., Ford, G., Gervais, A., Lacasse, Y., Maltais, F., Road, J., Rocker, G., Sin, D., Sinuff, T., Voduc, N. (2008). Canadian Thoracic Society recommendations for management of chronic obstructive pulmonary disease – 2008 update – highlights for primary care. Canadian Respiratory Journal, 15 Suppl A.
2. Global Initiative for Chronic Obstructive Lung Disease (GOLD) (2017). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. http://www.goldcopd.org
3. Stats Canada (2017). Canadian megatrends: Canada goes urban.
http://www.statcan.gc.ca/pub/11-630-x/11-630-x2015004-eng.htm
4. Jester, R.C & Malone, G.W. (2003). Respiratory Health on the Poultry Farm, Publication no.SF-8. National Ag Safety Database. Retrieved from http://nasdonline.org/197/d000146/respiratory-health-on-the-poultry-farm.html
5. Health & Safety Executive (HSE) (2009). Statement of evidence Respiratory hazards of poultry dust. http://www.hse.gov.uk/pubns/web40.pdf
6. Health & Safety Executive (HSE) (2008). Exposure to dust and bioaerosols in poultry farming: Summary of observations and data RR655. http://www.hse.gov.uk/research/rrhtm/index.htm
7. Heyder, J. (2004). Deposition of inhaled particles in the human respiratory tract and consequences for regional targeting in respiratory drug delivery. Proceedings of the American Thoracic Society. 1(4), 315-320. DOI: 10.1513/pats.200409-046TA
8. Canadian Centre for Occupational Health and Safety (CCOHS) (2012). How do particulates enter the respiratory system. https://www.ccohs.ca/oshanswers/chemicals/how_do.html
9. Kim, S.J., Im, J.G., Kim, I.O., Cho, S.T., Cha, S.-H., Park, K.S. & Kim, D.Y. (1995). Normal bronchial and pulmonary arterial diameters measured by thin section CT. Journal of Computer Assisted Tomography, 19(3), 365–369. https://www.ncbi.nlm.nih.gov/pubmed/7790543
10. Canadian Lung Association (2015). Chronic obstructive lung disease (COPD). Retrieved from https://www.lung.ca
11. Dosman, J.A., Senthilselvan, A., Kirychuk, S.P., Lemay, S., Barber, E.M., Willson, P., Cormier, Y., Hurst, T.S. (2000). Positive human health effects of wearing a respirator in a swine barn. Chest.118:852–860.
12. Canadian Standards Association (2011, reaffirmed 2016). Selection, use and care of respirators, Regulation. CSA, CAN/CSA-Z94.4-11.
13. National Institute of Occupational Safety and Health (NIOSH) (2014). Guide to the Selection and Use of Particulate Respirators. Centres for Disease Prevention and Control. https://www.cdc.gov/niosh/docs/96-101/default.html
14. Choinière, Y. & Munroe, J.A. (1997). Air quality inside livestock barns. Ontario Ministry of Agriculture, Food and Rural Affairs. http://www.omafra.gov.on.ca/english/livestock/swine/facts/93-001.htm

YATI Team, Halloween 2017
Youth as Social Change-Makers
By Donna Pan, Program Assistant, Youth Advocacy Training Institute
The Youth Advocacy Training Institute (YATI) is a unique program of The Lung Association that is funded by the Ministry of Health and Long-Term Care under the Smoke-Free Ontario Strategy (SFOS). YATI specifically works in tobacco control to reduce use amongst youth and young adults. We do this by adapting our trainings and events to meet stakeholder needs as both policy measures and the tobacco control community evolve. YATI works to equip youth, young adults, and professionals working with youth with the knowledge and skill base to further the SFOS goal for Ontario to have the lowest smoking rate in all of Canada.
It is crucial to understand why tobacco control must begin with our youth. One in five Ontario students have been reported to have tried a cigarette and 15.3 percent of all grade 12 students have used tobacco in the past year. Additionally, when focusing on youth within priority populations (Indigenous and LGBTQ2S youth), use of tobacco had some of the highest rates: 17 percent for those aged 20-24 and 23 percent for those aged 25-29 years old. These statistics in combination with the fact that two thirds of all youth who try cigarettes will go on to become regular smokers in their adulthood illuminates the need for targeted cessation efforts.
The Youth Advocacy Training Institute encourages youth to become leaders within their own communities, promote health and advocate for change. From education, awareness and training, to collaborating and capacity building with organizations across the province, to knowledge exchange opportunities, YATI has a plethora of services to offer. We strongly believe in a peer-to-peer and multi-faceted learning experience for our youth to gain the necessary knowledge. In addition, we focus on both a tobacco industry denormalization and a youth engagement lens. Since 2005, YATI has reached more than 40,000 youth, young adults, and adults across Ontario. As we work directly with youth, it is critical that we continue to be easily adaptable to these evolving areas of tobacco policy in order to maintain our pivotal role as one of five knowledge centres within the province.
As the name suggests, one of YATI’s central focuses are the trainings offered across the province for public health units and community organizations. Trainings are offered under two age categories – youth and young adults from ages 12-24 and adults aged 25+. The trainings are free of cost, offered in both English and French, and are facilitated with a combination of both adult and young adult trainers. Our youth trainings are designed to support youth with the tools and skills crucial to becoming advocates within their communities. Training programs available for youth include Plain and Standardized Packaging: Plain and Simple, Walking the Good-Life (Mino-Pimatisiwin), Tobacco 202: Emerging Issues, Tobacco Industry Denormalization, and many more! On the other hand, our adult trainings are meant for professionals who work with youth and want to further develop their youth engagement skills in order to provide the necessary support needed for positive development. Some adult trainings offered include Youth Social Identities and Health Promotion, Social Media and #HealthPromotion, Promising Practices in Youth Tobacco Cessation and Engage 2.0 Principles and Practises of Meaningful Youth Engagement.
Walking the Good-Life (Mino-Pimatisiwin) is a distinct training program that gained popularity this past year. It promotes awareness on prevalent issues within Indigenous communities regarding the impact of colonization on tobacco from both a traditional and commercial perspective. This training allows youth within these local communities to address the issues surrounding the industrialization as well as commercialization of tobacco. This training was recently spot-lighted in The Dryden Observer where one youth stated that while they live in an Indigenous community, a lot of them had very little knowledge on the history of sacred and traditional tobacco. In order for these youth to become advocates, this awareness around the exploitation of natural and sacred tobacco must be taught.
The Youth Advocacy Training Institute also has a role in addressing youth trends related to emerging tobacco control issues. E-cigarettes have been gaining immense popularity and while the majority of users are adults, about 20 percent of youth ages 15-19 have reported to have used e-cigarettes. Shockingly, this statistic includes the 14 percent of youth who do identify as non-smokers. This illuminates the strong correlation between e-cigarette users and those who move on to become cigarette smokers. A new study found that 10 percent of the youth studied had used e-cigarettes in the past 30 days – a stark increase from three percent in 20131. With that said, youth who have smoked e-cigarettes in the past 30 days were more likely to take up cigarette smoking which then led to an increase in those who smoked daily. This growth in popularity within the youth demographic, demonstrates that e-cigarettes may be a way to normalize smoking. While there is need for more research about e-cigarettes and their potential as a cessation aid, the research is clear that we do not want young people, especially those who don’t smoke, to start.
The Youth Advocacy Training Institute also plays a critical role in reducing youth tobacco use by supporting those who smoke to quit. One significant way we have achieved this is through the pilot launch of the Not On Tobacco (NOT) cessation program, originally developed by the American Lung Association (ALA). This is a voluntary program based within high schools for students ages 14-19 who identify as daily smokers and are motivated to quit. Adult allies assist youth over a period of 10 weekly sessions that are 50 minutes in length by facilitating programs that use different strategies to help them develop the skills and confidence needed to quit. This was piloted in more than 11 schools in Ontario from 2014 to 2017, with more programs scheduled to run in early 2018. The ALA’s NOT program has been modified for Ontario settings which includes implementing youth engagement strategies into the curriculum as well as adapting the evaluation tool and facilitation model. Over the course of the three years, 109 youth participated in the pilot programs where 12 percent of those who responded to the end of program survey had quit smoking. Those who did not quit and continued to smoke were smoking less than before from an initial average of 12 cigarettes a day during the week to 6.1 cigarettes at the end of the program. The YATI is proud to pilot a program that is working to significantly reduce cigarette consumption amongst youth as well as play a role in changing the way youth smokers think about smoking patterns and encourage them to take action to quit on their own.
The Youth Advocacy Training Institute’s core values and practices lie within youth engagement. Ultimately, we work to engage youth at every level as this framework successfully supports youth to become advocates in health promotion and tobacco control. By focusing on youth to become these change-makers is how we can meet the Smoke-Free Ontario Strategy vision together.
1 Hammond, D., PhD, Reid, J. L., MSc, Cole, A. G., MSc, & Leatherdale, S. T., PhD. (2017). Electronic cigarette use and smoking initiation among youth: a longitudinal cohort study. CMAJ, 189(43), E1328-E1336. doi:10.1503

Helping Kids Stay Active and Healthy
After school programs across several regions are running, jumping and competing in relays to learn about Asthma and healthy lungs! Play for All is an innovative program that combines education on lung health and asthma awareness in a fun, interactive environment to help kids stay healthy and active. Participants learn the health-related benefits of physical activity especially for lung health.
 The Lung Association – Ontario is pleased to be partnering with Boys and Girls Clubs in Hamilton, Scarborough, York Region and Durham Region during the 2017-18 school year on the delivery of this after school program. The program hopes to train more than 40 staff and reach 700 to 800 students between grades one through six. Play for All provides an opportunity for these children to learn in an environment that is comfortable, inclusive and engaging. It provides hands-on experience through lung health activities, and the participants have the opportunity to engage family and friends in what they are learning.
The Lung Association – Ontario is pleased to be partnering with Boys and Girls Clubs in Hamilton, Scarborough, York Region and Durham Region during the 2017-18 school year on the delivery of this after school program. The program hopes to train more than 40 staff and reach 700 to 800 students between grades one through six. Play for All provides an opportunity for these children to learn in an environment that is comfortable, inclusive and engaging. It provides hands-on experience through lung health activities, and the participants have the opportunity to engage family and friends in what they are learning.
Asthma is a chronic disease. About one in five children have asthma. Regular physical activity is important to the health and well-being of all children. Yet children who have asthma and their families often see asthma as a barrier to being physically active. There is growing evidence in the literature to show that activity levels among children and youth with asthma are lower than their peers without asthma. Poorly controlled asthma can limit a child’s ability to play, exercise, and sleep — all critical to his or her development. Uncontrolled asthma can also lead to a child withdrawing from physical activity and sport. When asthma is well managed and well controlled, however, children who have asthma should be able to participate fully in all activities.
The Play for All program goals are to:
- encourage children with asthma to become physically literate and active for life;
- improve children’s understanding of lung health and the role of physical activity in maintaining it;
- improve parents’ understanding and comfort level with their child’s participation in physical activities;
- provide a supportive and safe exercise environment; and to
- build the capacity of the community recreation sector to support children with asthma.
- The Play for All program is comprised of staff training, program implementation, parent engagement and evaluation. The program has 25 different lung health activities
- that are completed with the children over a 12-week period. These activities are divided into five different lung health sections.
L – look after them (Asthma & Lungs)
U – use them (Physical Activity & Lungs)
N – nurture them (Healthy Eating & Lungs)
G – guard them (Air Quality & Lungs)
S – save them (Tobacco Wise & Lungs)
This will be the third year the Play for All program has been offered in partnership with Boys and Girls clubs, and to date, the feedback from staff, participants and parents has been positive. During the 2016-17 school year, 83% of participants strongly agreed or agreed that the Play for All program helped them to understand asthma, including asthma symptoms, triggers and resources and 82% of participants strongly agreed or agreed that the program helped them to understand the importance of physical activity for lung health.
The parents seemed equally pleased, as 91% of them strongly agreed or agreed that the program was a positive experience for their child, and 93% of the parents strongly agreed or agreed that staff were knowledgeable about asthma including asthma symptoms, triggers and resources.
“My lungs are healthy because I exercise and eat healthy food!” – child
“I loved the games and learning about asthma.” – child
“I liked Play for All because it helped others learn about my child’s asthma.” – parent
“This was a great way to have the kids learn and play at the same time.” – staff
In addition to educating kids about their lung health, the program also trains staff on signs and symptoms of asthma and how to help children with asthma manage their attacks. This gives the staff, parents and children with asthma more confidence to participate in physical activities with the other children.
The Lung Association – Ontario is pleased to be a partner in a program that encourages healthy lungs and healthy lifestyle choices for children.
For more information about the Play for All program or for additional resources on asthma or lung health, please visit The Lung Association – Ontario website at: www.lungontario.ca, or email info@lungontario.ca, or call The Lung Health Information Line at 1-888-344-LUNG (5864).
Get Involved

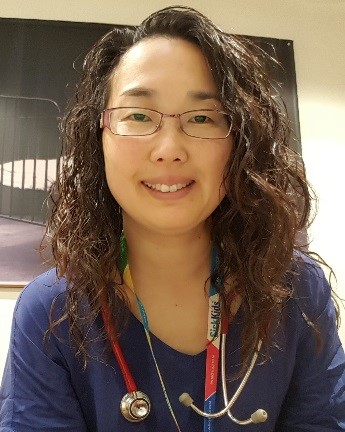
SHELLEY PREVOST
is a respiratory therapist at St. Joseph’s Care Group in Thunder Bay. In this role, she has developed an evidence-based pulmonary rehabilitation program, an in- and outpatient chronic assisted ventilation program for adults requiring long-term chronic ventilation, and a COPD Education Clinic. She has also spearheaded a number of research projects, has presented at numerous conferences, has been interviewed by various media sources, and has been published in peer-reviewed publications.
Shelley is a lifelong learner, holding a respiratory therapy diploma, a Bachelor of Business, a COPD Educator Certificate (2003), a Masters of Respiratory Science (2010), and an Asthma Educator Certificate (2017).
She is highly committed to professional excellence, as demonstrated by her active involvement in organizations associated with professional practice. Since 2013 she has been involved with the ORCS in a number of capacities, most notably as Chair from 2014-2016. Prior to taking on this role, she sat on the Northwestern Ontario Regional committee and served as a longstanding member of the Respiratory Health Educators Interest Group (RHEIG). She has also been an active member of the Respiratory Therapy Society of Ontario (RTSO), sitting on the Research and Community Respiratory Therapy committees. In addition, Shelley has reviewed proposals for the Canadian Society of Respiratory Therapists and been involved in the “Every Breath Counts Lung Health Support Group” as both a founder and speaker. She also somehow finds the time to be involved in the Children’s Aid Society of Thunder Bay, the Thunder Bay Christmas Cheer Fund and Habitat for Humanity.
Her leadership abilities are bolstered by her exceptional communication and interpersonal skills, enthusiasm, dependability, and high moral standards. She also demonstrates outstanding critical thinking, focus, analytical and problem solving abilities.
Shelley’s commitment to exemplary clinical practice and lifelong learning, alongside her contagious enthusiasm and seemingly limitless energy, significantly improves respiratory care in Ontario.
Research and Fellowship Awards
ORCS Research & Fellowship Committee Chair, Mika Nonoyama, PhD, Assistant Professor, Registered Respiratory Therapist
Research Grants and Fellowship Awards support research and graduate study by health-care providers in the field of respiratory care. The objective of this fund is to promote research regarding any field of acute or chronic lung disease. Research may include investigation of any phenomenon pertinent to illness assessment, management, or responses of the individual with a respiratory condition. Research may also be aimed at health promotion, education and prevention issues. Studies may use quantitative or qualitative methodologies.
The Lung Association – Ontario is committed to supporting the best respiratory research in Ontario. The Lung Association has established focus areas: asthma, air quality and smoking-related lung disease. Projects in these areas are encouraged. However, the primary criterion for the awarding of research monies shall be the excellence of the research proposal.
Click here to access the grant and fellowship guidelines and applications. (https://lungontario.ca/for-health-professionals/ontario-respiratory-care-society/research/)
Common Asthma Triggers: An Education Companion
The Primary Care Asthma Program (PCAP) is an evidence-based, standardized program model under the Ministry of Health and Long-Term Care (MOHLTC) Asthma Program. The program currently includes standardized asthma and COPD tools through a partnership with The Lung Association – Ontario (TLA). PCAP is delivered within a multi-disciplinary team of providers led by a Certified Respiratory Educator (CRE) across Ontario. In 2014, PCAP partnered with the MOHLTC to conduct a needs assessment using the MOHLTC Health Equity Impact Assessment (HEIA)1 to identify how PCAP was impacting their population groups and to ensure more equitable delivery of the program including its service, policy and tools, and to align with the National Lung Health Framework2 goals.
Ten PCAP coordinators across Ontario completed the MOHLTC HEIA and results were presented to TLA. Out of the six impacted populations identified by PCAP, TLA decided to produce asthma resources that addressed low literacy and language barriers. In 2016, a pictorial triggers booklet was developed for educators to use with their patients with low literacy or English as a second language titled, Common Asthma Triggers: An Education Companion. This is a three-fold tool that will help these patients to identify and communicate their triggers to their clinicians.
As Ontario moves towards a health-care system designed around the patient as detailed in the Patients First Act 2016, it will be important to continue to design and improve programs, policies and tools to address the social, economic, environmental and cultural determinants of health for the patient.
To order/download a copy, call The Lung Association at 1-888-344-5864, email info@lungontario.ca or go to www.lungontario.ca.
UPCOMING EVENT LISTINGS
January 13-14, 2018
Toronto
RESPTREC™ Asthma Module
RESPTREC™ offers courses for those who wish to pursue their Certified Respiratory Educator designation. The Education module remains the foundation for learning how to engage patients in self-management. Learners will learn how to apply educational theory to practice. The Asthma and COPD modules are disease-specific courses based upon the most recent evidence-based published guidelines and references for disease management.
January 18 – 21, 2018
Toronto
RESPTREC™ COPD Module plus education
RESPTREC™ offers courses for those who wish to pursue their Certified Respiratory Educator designation. The Education module remains the foundation for learning how to engage patients in self-management. Learners will learn how to apply educational theory to practice. The Asthma and COPD modules are disease-specific courses based upon the most recent evidence-based published guidelines and references for disease management.
January 24-25, 2018
Respiratory Health Forum
The Lung Association Primary Care Asthma Program will be holding a Respiratory Health Forum at the Marriott Toronto Downtown Eaton Centre prior to The Lung Association’s annual Better Breathing Conference.
Spirometry Interpretation Workshop
Provider Education Program’s Spirometry Interpretation Accredited Workshop will take place at the Respiratory Health Forum on Wednesday, January 24th, 2017 from 2:00pm to 4:15pm.
To register, visit: https://lungontario.ca/for-health-professionals/educational-opportunities/respiratory-health-forum-registration/
January 25, 2018
Breathe! Gala
Save the date! Join The Lung Association – Ontario for an evening of celebration and help us continue to create breathing breakthroughs!
January 25-27, 2018
Better Breathing Conference
Better Breathing 2018 will be held at the Marriott Toronto Downtown Eaton Centre Hotel, presented by two professional societies: Ontario Thoracic Society (OTS) & Ontario Respiratory Care Society (ORCS). New this year will be a Respiratory Therapy Society of Ontario (RTSO) education program featuring acute and community sessions, as well as the RTSO sponsored poster session and cocktail reception. www.betterbreathing.ca
February 26-March 9, 2018
Breath of Spring Campaign (Formerly Tulip Day)Purchase tulips and crispy wave ferns and help more Canadians breathe easy by funding lifesaving lung research. For more information and ways to get involved, please visit the Breath of Spring website.
March 3, 2018
Toronto
RESPTREC™– SPIROTrec – 1 day course
RESPTREC™ offers courses for those who wish to pursue their Certified Respiratory Educator designation. The Education module remains the foundation for learning how to engage patients in self-management. Learners will learn how to apply educational theory to practice. The Spirometry course is a one-day module that focuses on the skills and knowledge required to conduct quality spirometry based upon the most recent guidelines.
March 13, 2017
Respiratory Medications and Devices: What You Need to Know
The Lung Association – Ontario’s Provider Education Program will be running a workshop on Respiratory Medications via OTN, 12:00-13:00. For more information and to register, please visit http://olapep.ca/
Check http://olapep.ca/ for the upcoming Provider Educator Program OTN webcasts on Pulmonary Rehabilitation for COPD and Asthma and Allergies.
March 22 – 25, 2018
Toronto
RESPTREC™ COPD Module plus education
RESPTREC™ offers courses for those who wish to pursue their Certified Respiratory Educator designation. The Education module remains the foundation for learning how to engage patients in self-management. Learners will learn how to apply educational theory to practice. The Asthma and COPD modules are disease-specific courses based upon the most recent evidence-based published guidelines and references for disease management.
April 21 – 22, 2018
Toronto
RESPTREC™ Asthma Module
RESPTREC™ offers courses for those who wish to pursue their Certified Respiratory Educator designation. The Education module remains the foundation for learning how to engage patients in self-management. Learners will learn how to apply educational theory to practice. The Asthma and COPD modules are disease-specific courses based upon the most recent evidence-based published guidelines and references for disease management.
May 26 – 27, 2018
Ottawa
RESPTREC™ COPD Module only
RESPTREC™ offers courses for those who wish to pursue their Certified Respiratory Educator designation. The Education module remains the foundation for learning how to engage patients in self-management. Learners will learn how to apply educational theory to practice. The Asthma and COPD modules are disease-specific courses based upon the most recent evidence-based published guidelines and references for disease management.
EDITORIAL Committee
CO-CHAIRS
Jocelyn Carr, BScPT, MSc
Lorelei Samis, BScPT
MEMBERS
Yvonne Drasovean, RRT
Elizabeth Gartner, BScOT
Therese Hawn, BScPT
Lawrence Jackson, BScPhm
Priscila Robles, BScPT, MSc, PhD
CHAIR, ONTARIO RESPIRATORY CARE SOCIETY
Dina Brooks, BScPT, MSc, PhD
PRESIDENT & CEO, THE LUNG ASSOCIATION – ONTARIO
George Habib, BA, BEd, CAE
DIRECTOR, ONTARIO RESPIRATORY CARE SOCIETY
Sherry Zarins
OTS/ORCS Coordinator
Natalie Bennett
RHEIG Executive Team
CO-CHAIRS
Jane Lindsay, BScPT, CRE
Lorelei Samis, BScPT
MEMBERS
Cassy Bernard, RN
Lana Biro, RRT, CRE
Karen Brooks, RN, BSc, CRE, CTE
Michael Callihoo, RRT, CRE
Rose-Marie Dolinar, RN(EC), MScN, PhD student
Diane Feldman, RRT, CRE
Olivia Ng, BScPhm, RPh, PharmD (Candidate)
Maria Willms, RN, CRE
Rebecca Whiting, RRT, CRE
An official publication of the Ontario Respiratory Care Society, a section of The Lung Association.