Prior to 2020, the Lung Health Foundation operated as the Ontario Lung Association. Enjoy this content from our archives.

An official publication of the Ontario Respiratory Care Society, a section of the Lung Health Foundation
Update on Respiratory Health, Research and Education is a publication of the Ontario Respiratory Care Society, a section of the Lung Health Foundation. Update is published three times per year and includes peer-reviewed original articles, clinical practice tools, health news, and communications between the ORCS and its membership.

CHAIR’S MESSAGE
I’m very excited to be writing my first Chair’s message for Update on Respiratory Health, Research and Education! Firstly, I’d like to thank Dina Brooks, BScPT, MSc, PhD, our new Past-Chair, for her dedication and commitment to the Ontario Respiratory Care Society (ORCS) for more than 25 years, and to congratulate her on her new role at McMaster as Vice Dean (Health Sciences) and Executive Director, School of Rehabilitation Science. I also want to acknowledge Ann Bartlett, RN, MSc, BScN, CRE, who is retiring from St. Joseph’s Healthcare, Hamilton after more than 41 years of service. Ann has been an ORCS member since 2001. She was very active with ORCS. She represented the South Central Region on the Provincial Committee and played a leadership role on both the Education Committee and the Respiratory Health Educators Interest Group (RHEIG). We wish both Dina and Ann all the best for these new directions in their lives.
Personally, I have been working in the respiratory field for almost 40 years as a respiratory therapist and have been an ORCS member since the mid 80’s. (Don’t bother with the math!) I truly have a passion for the profession of respiratory therapy and believe strongly in the value of being an active member of the ORCS. I’ve said before that the cost of not becoming a member is far greater than the cost of becoming a member. The collaboration, the networking, the opportunities to learn and to grow can’t be beat, and, for students, membership is free. New this year, ORCS membership is no longer included in RTSO membership. So if you haven’t renewed your ORCS membership yet for 2019-2020, do so today at http://lungontario.ca/for-health-professionals/ontario-respiratory-care-society/.
This issue of the ORCS Publication features a wide variety of articles, including Internet Mediated Research, Quality Improvement in Respiratory Care, and Medical Assistance in Dying (MAiD). Our In the Spotlight features winners from the Poster Session at the Better Breathing Conference 2019, which was held January 24 – 26 at the Toronto Marriot Downtown Eaton Centre. Led by Education Committee Chair, Mike Keim, planning has already started for Better Breathing 2020! If you have thoughts/recommendations on topics and speakers for next year and beyond, don’t hesitate to send them to: societies@lungontario.ca.
Our ORCS members are very important to us; without membership we do not have an ORCS! The ORCS has been in existence for more than 25 years and we are committed to keeping it relevant to its members. To live that commitment, we undertook a comprehensive review of our member benefits and educational opportunities to ensure we have a good understanding of what matters most to our members. The survey was fielded to approximately 1,400 current and lapsed members in mid-March. I am thrilled to share a few of the key results gained. In terms of member engagement and opportunities: 60% of members indicated that their membership has provided opportunities for networking and 25% of members indicated that their membership has help to improve their job opportunities. In terms of ongoing professional education: 73% of members reported that they have received meaningful professional development opportunities through their membership, 81% of members indicated that ORCS educational events provided a meaningful professional development opportunity, and 78% of members indicated that they are likely to attend ORCS educational programs in the year ahead. Many thanks to those that completed the survey and for providing us with this very important data.
Don’t forget to save the date for Better Breathing 2020! January 23 – 25, 2019.
Respectfully submitted,
Miriam Freymond Turnbull, MBA, RRT
Chair, Ontario Respiratory Care Society.

EDITOR’S MESSAGE
In my first Editor’s message allow me to express my gratitude and excitement for being part of this wonderful community of caring people. There is nothing I find more empowering, engaging and motivating than learning from passionate individuals in the field of respiratory care, from novice to experts and our patients, who believe in the importance of continuing education. In a world where digital distractions put us all at risk of losing focus, sharing informative and relevant knowledge can and will help us stay the course in our professional quest to improve respiratory care.
The year started with an excellent Better Breathing Conference in January, continuing with exciting plans for improvement and renewal. While the season is changing, with flowers blooming and temperatures rising, inviting us to enjoy fun outdoor activities, let’s not lose the momentum and continue to engage one another in the world of continuous education in respiratory care. In this spring 2019 edition of Update on Respiratory Health, Research, and Education, we invite you to discover news, learning opportunities, and ideas for future contributions to our community of learning. Our first feature article has been written by Sue Jones and provides an excellent review of quality standards in respiratory care, highlighting their importance as resource for practitioners and patients. In the second feature article, Julie Duff Cloutier presents current research on Internet Mediated Research (IMR) in Clinical Practice. This edition of our publication also offers new perspectives on medically assisted dying, including emerging trends in the acute care settings with an article written by Dr. Debbie Selby and Sally Bean. Along with informative summaries of articles we think might interest you, a presentation of the 2019 Better Breathing Conference poster presentations winners is also available in our In the Spotlight section. Last but not least, Peter Glazier offers a review of the Lung Health Foundation’s annual fundraiser Breathe!Bash
As we provide you with this electronic publication we hope to engage you with the content and challenge you to analyze the information. We also look forward to hearing from you on the content of future editions.
Sincerely,
Yvonne Drasovean BSc, RRT, FCSRT, MEd
Co-chair Editorial Board
Internet-mediated research: Application to Clinical Research
By: Julie Duff Cloutier, RN, MSc, PhD(c)
Laurentian University, School of Nursing, School of Rural and Northern Health
In my first Editor’s message allow me to express my gratitude and excitement for being part of this wonderful community of caring people. There is nothing I find more empowering, engaging and motivating than learning from passionate individuals in the field of respiratory care, from novice to experts and our patients, who believe in the importance of continuing education. In a world where digital distractions put us all at risk of losing focus, sharing informative and relevant knowledge can and will help us stay the course in our professional quest to improve respiratory care.
What is Internet-mediated research?
Accompanying this health and social trend is the evolution of internet-mediated research (also known as online research) over the past decade. Internet-mediated research is broadly defined as identifying, gathering and analyzing novel and original data for the purpose of generating knowledge relative to a focused inquiry (3). Internet-mediated research is characterized as pragmatic and has expanded across a diverse range of disciplines over the past decade (2, 4). Internet-mediated research methods are very diverse. They are used across the social science disciplines and effectively produce data, whether directly elicited or not. Data may be numeric, graphical, textual, or in audio-visual formats (2). The contexts in which data are produced vary from tightly designed experiments to more naturalistic approaches. As such, internet-mediated research has developed in the area of health research. In health research, the systematic ‘mining’ of information may involve the extraction of either objective or subjective text from online repositories to yield quantitative and/or qualitative results.
Why is Internet-mediated research an appropriate and practical method to use?
The use of digital technologies is not new to health research. Many health researchers interact with data services online and have access to existing data files in a serviceable form. One of the main advantages of internet-mediated research methods is its pragmatic focus. Most of us already make an attempt to reuse what we produce in our everyday lives. With internet-mediated research methods, it is the same idea but further applied to data, or information that is available as potential data. This supports pragmatism. Pragmatism focuses on the practical and the achievable- a notion that many of those working in health research would support (5, 6). Pragmatism describes knowledge as a tool for action and as such, it must be rigorously evaluated according to whether it addresses the topic of study. A pragmatist’s approach to knowledge becomes, “How does this knowledge serve our purpose?” It accepts a variety of competing interests and forms of knowledge (7). From a research perspective, perfect knowledge is not possible nor required because knowledge is only meaningful when coupled with action. As such, internet-mediated research is pragmatic in its approach to how we use available information to gain knowledge within a certain area. Another key feature of pragmatism is the contextualization of knowledge (5). As contexts change, so does the usefulness of knowledge. Again, this is applicable to internet-mediated research as information gathered from online sources is context bound. In addition, analysis and discussion would also include this concept.
The evolving internet presents health researchers with new opportunities that may lessen the challenges of some traditional methods. For example, internet-mediated research is cost- and time-efficient and allows access to large data sources. If one were to use traditional research methods, this type of data would only be available to primary researchers of funded and group administrated surveys. Such funding is often difficult for novice researchers to access. Furthermore, internet-mediated research methods allow persons greater freedom through networking where they can interact with information or others, at their convenience (4, 8-10). Some authors have also suggested that online users may have higher levels of candor and self-disclosure compared to traditional research methods, which may reduce social desirability bias effects. The nature of the online data collection can also provide a built-in audit trail (4, 11, 12).
Although there are many advantages, internet-mediated research is not without its challenges. In quantitative studies, disadvantages of this method are related to the reliability and validity of quantitative data (4). However, in most of the studies, the reduced level of researcher control in secondary analyses of existing data is comparable to secondary analyses of existing offline data. In qualitative studies, disadvantages of this method for the qualitative data components relate to trustworthiness (4). A somewhat unique disadvantage specific to internet-mediated research methods is the vastness of data that can accumulate in quantity quickly. Researchers must realise that the initial form of the data is rarely the form that yields useful information (13). Data must be organized to make them useful.
Why is Internet-mediated research particularly applicable to the clinical population of persons who live with respiratory illnesses?
Persons living with respiratory illness may welcome the opportunity to participate in online research studies compared to traditional research methods as they may complete forms, surveys, or describe their experiences during times and locations where it is convenient for them. The readily available interactive mediums available online offer the possibility of conversing without the obstacle of breathlessness or geography. In addition, the internet promotes access to hard-to-reach persons or communities (Paige, Stellefson, Chaney, & Alber, 2015). In conclusion, there are interesting times ahead as the world of internet-mediated research continues to develop.
References
- Statistics Canada. Life in the fast lane: How are Canadians managing?. The Daily, 2017 (11), 3.
- Lee RM, Fielding NG, & Blank G. Online research methods in the social sciences: An editorial introduction. In Fielding NG, Lee RM, & Blank G. (eds.). The sage handbook of online research methods. (2nd). London: Sage Publications. 2017 3-16.
- Hewson C, Yule P, Laurent D, & Vogel CM. Internet research methods: A practical guide for the social and behavioural sciences. London: Sage Publications. 2003
- Hewson C. Research design and tools for online research. In Fielding NG, Lee RM, & Blank G. (eds.). The sage handbook of online research methods. (2nd). London: Sage Publications. 2017 57-75.
- Long K M, McDermott F, & Meadows GN. Being pragmatic about healthcare complexity: our experiences applying complexity theory and pragmatism to health services research. BMC Medicine, 2018 16(1). org/10.1186/s12916-018-1087-6
- Deforge R, & Shaw J. Back-and-fore-grounding ontology: exploring the linkages between critical realism, pragmatism, and methodologies in health and rehabilitation sciences. Nurs Inq, 2012 19(1), 83-95. doi:10.1111/j.1440-1800.2011.00550.x.
- Cornish F& Gillespie A. A pragmatist approach to the problem of knowledge in health psychology. J Health Psyc, 2009 14(6), 800-809. doi:10.1177/1359105309338974.
- Merolli M, Gray K, & Martin-Sanchez F. The outcomes and related effects of using social media in chronic disease management: A literature review and analysis of affordances. J Biomed Info, 2013 46, 957-969.
- Paige S, Stellefson M, Chaney BH, & Alber JM. Pinterest as a resource for health information on chronic obstructive pulmonary disease (COPD): A social media content analysis. Amer J Health Educ, 2015 46, 241-251. doi:10.1080/19325037.2015.1044586.
- StellefsonM, Shuster JJ, Chaney BH, Paige SR, Alber JM, & Chaney D. Web-based health information seeking and ehealth literacy among patients living with chronic obstructive pulmonary disease (COPD). Health Commun, 2018 33(12), 1410-1424. doi:10.1080/10410236.2017.1353868.
- Joinson A & Payne CB. ‘Self-disclosure, privacy and the Internet”. In Joinson A McKenna K Postmes T Reips UD. (eds). Oxford Handbook of Internet Psychology. Oxford: Oxford University Press, 2007 235-250.
- Wilson E, Kenny A, & Dickson-Swift V. Using blogs as a qualitative health research tool: A scoping review. Inter J Qual Methods, 2015 14(5). org/10.1177/1609406915618049.
- Blank G. Online research methods and social theory. In Fielding NG, Lee RM, & Blank G. (eds.). The sage handbook of online research methods. (2nd). London: Sage Publications. 2017 628-641.

COPD Quality Standards
Submitted by Sue Jones, RRT, NFCSRT, LSSBB, QI Specialist, Health Quality Ontario
Background
Quality Standards are created for conditions that show large variations in care delivery among care providers and facilities with identified gaps between provincial standards of care and actual care provided.
Quality Standards are grounded in best practice evidence and are designed to:
- Help patients, residents, families, and caregivers know what to ask when they visit their provider;
- Help healthcare professionals know what care to offer, based on evidence and expert consensus;
- Help healthcare organizations measure, assess, and improve the quality of care they provide and;
- Help ensure consistent, high quality care across the province.
Each Quality Standard includes a set of resources for providers and patients, including:
- A patient guide for patients, families and caregivers to help structure the discussion about their care with their healthcare professionals.
- An information briefwith data on how care is being
delivered for that condition in Ontario, and the variations in care, to
help people understand why a quality standard has been created. - Data and a measurement guidefor healthcare professionals and organizations to help collect feedback on their quality improvement efforts.
- Recommendations for adoptionthat acknowledge the
barriers and prioritize actions at the system, regional and practice
levels to help healthcare professionals and organizations adopt the
standards. The Getting Started Guide is available and provides additional practical tools for quality improvement.
Each Quality Standard is developed with input from a broad range of stakeholders from across the province, including patients and healthcare providers. They are designed to become a resource for organizations, care teams and other health system partners to drive quality improvement efforts by using the standards as they plan their quality improvement initiatives.
Why a Chronic Obstructive Pulmonary Disorder (COPD) Quality Standard?
Despite a decrease in the smoking rate, COPD is the leading cause of morbidity and mortality worldwide. Prevalence of COPD continues to increase and now sits at 11.8% of Ontarians in 2015. However, only 40% of those living with COPD receive spirometry confirmed diagnosis.
COPD is the second most common reason for hospitalization in Ontario, with an economic burden and direct costs estimated to be $3.3 billion worldwide
The Quality Statements in the COPD Quality Standard include:
|
|
Quality Standards vs Quality Based Procedures
Quality Standards support Quality Based Procedures (QBPs) by providing evidence based recommendations to improve care. For example, in the COPD QBP, post-acute phase Pulmonary Rehabilitation is part of the plan for moderate to severe COPD patients. One of the challenges we face in Ontario is equal access to such programs. The Quality Standards include a statement about the criteria and use of pulmonary rehabilitation programs to improve quality of life. It also acknowledges that access to pulmonary rehabilitation programs are limited as a structural indicator. Both the Quality Standard and the QBP align in providing evidence that follow-up appointments reduce emergency department visits and readmission rates.
Using Quality Standards
Starting the implementation journey can be challenging. Recommendations for Adoption (RFA) are an integral part of the quality standards program. They are intended to aggregate and acknowledge barriers that are in place at the system level and make recommendations to various system partners to address these barriers. Therefore, the RFA and Quality Standard statements can be considered complementary documents. The Quality Standards Getting Started Guide is also available to help organizations and healthcare professionals assess which quality statements should be prioritized for quality improvement efforts.
Working alone can be daunting so it’s best to consider creating a regional collaborative group and include stakeholders from acute care, primary care, long term care, telehomecare, home & community care, community paramedicine, home oxygen companies, palliative care, and local community pharmacists. With this collaborative group, use a Quality Improvement methodology that includes: Creating problem statements and aim statements, brainstorming change ideas, testing the change ideas using PDSA cycles and making adjustments as needed. Use tools such as a fishbone, process mapping and the 5 whys to conduct a root cause analysis. Be bold and engage patients, families and caregivers in your design. Lastly, create measures using the Quality Standards for COPD and implement locally meaningful data collection methods to promote evaluation.
How do we measure success as a local region and as a province?
At the local level, it may be possible to measure success of implementation of the Quality Standard using your own clinical records, or you might need to collect additional data. We recommend the following indicators to measure the quality of care patients are receiving:
- Percentage of people with COPD whose disease has a low or medium
impact on their life (stratification: low, medium, high, and very high
impact) - Percentage of people with moderate to severe COPD who have access to
a pulmonary rehabilitation program (stratification: community-based and
inpatient rehabilitation)
These indicators cannot be measured provincially using current available data sources.
At a system level, the following indicators can be used to measure overall success of the quality standard:
Process indicators:
- Percentage of people with COPD whose diagnosis is confirmed by spirometry
- Percentage of people hospitalized for COPD who had an in-person follow-up assessment with a physician within 7 days of discharge
- Percentage of people with COPD who have filled a prescription for
long-acting bronchodilator therapy (measurable for people aged 65 years
and older only)
Outcome indicators:
- Percentage of people with COPD with one or more urgent acute-care visits for COPD in the past year: Emergency department visits or Non-elective hospitalizations
- Percentage of people with COPD who smoke cigarettes daily
The use of evidence-based standards will improve care across the province, create equity and reduce variation in care. The Quality Standards take a holistic approach, including assessment, treatment, ongoing follow up, and prevention of worsening symptoms. It provides clinicians with a fulsome strategy while incorporating pieces that already exist in all practices. The key is to understand the statements, do your own gap analysis in your organization and create a plan to address the gaps.
All resources listed above can be found on the Health Quality Ontario website: https://www.hqontario.ca/Evidence-to-Improve-Care/Quality-Standards
References
- Gershon AS, Mecredy G, Ratnasingham S. Chronic Obstructive Pulmonary Disease in Ontario, 1996/97 to 2014/15. Toronto, ON: Institute for Clinical Evaluative Sciences; 2017. Available from: https://www.ices.on.ca/Publications/Atlases-and-Reports/2017/COPD
- The Ministry of Health and Long Term Care.Smoke-free Ontario: The next chapter – 2018. Kingston, Queens, 2018. Available from: http://www.health.gov.on.ca/en/common/ministry/publications/reports/SmokeFreeOntario/SFO_The_Next_Chapter.pdf
- University of Waterloo [Internet]. Waterloo: The University. Tobacco use in Canada; 2017. Available from: https://uwaterloo.ca/tobacco-use-canada/adult-tobacco-use/smoking-provinces/ontario
IN THE SPOTLIGHT
In the Spotlight features winners from the Poster Session at the Better Breathing Conference 2019, which was held January 24 – 26 at the Toronto Marriot Downtown Eaton Centre.
The winner of the Margaret Fitch award for best poster was Mika Nonoyama from the University of Toronto for her poster “Novel Device to Improve Airway Intubation Safety by Providing Apneic Oxygenation and On-demand Suction through the Endotracheal Tube: Piglet Protocol.” Co-authors were Mark Tessaro, Diane Soares, Cengiz Karsli, Thomas Looi, Alex Gordon.
The Lisa Cicutto award for best poster by a student was presented to Sachi O’Hoski of McMaster University for her poster “Reliability and Validity of a Measure of Participation in People with Chronic Obstructive Pulmonary Disease.” Co-authors were Ayse Kuspinar, Julie Richardson, Joshua Wald, Marla K Beauchamp.
The winner of the Sheila Gordon-Dillane award for best poster for program evaluation was Jacky Au, with co-authors Sarah Isaac, Renee Jensen, Sanja Stanojevic, and Felix Ratjen from The Hospital for Sick Children, for their poster “Improving Multiple Breath Washout Training Evaluation of E-learning Modules.”
Congratulations to all of our poster award winners!
We look forward to seeing you all at Better Breathing 2020!
Mark your calendars for January 23 – 25, 2020.
TOOL BOX

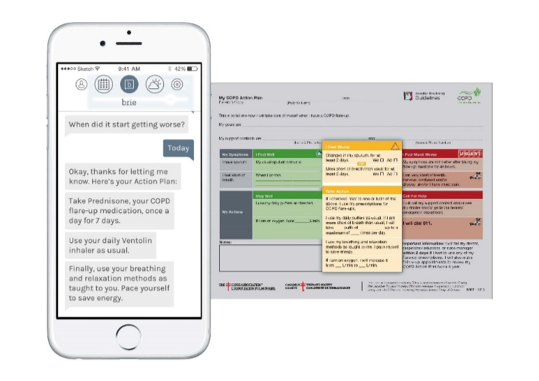
The Breathe App for Chronic Obstructive Pulmonary Disease (COPD)
Submitted by Aisha Balasubramaniam, MPH, RRT, CRE
COPD’s burden on healthcare and the individuals affected makes it an undeniable priority in regard to development of self-management options for patients, clinicians and medical institutions. Breathe for COPD transforms the current methods for the self-management of COPD, from a generic paper-based approach to one that is dynamic and personalized. The mobile app (currently optimized for iOS) enables patients to manage their exacerbations more efficiently and effectively.
As a “digital educator,” Breathe for COPD empowers patients to independently identify changes in their breathing. When the patient inputs their symptoms, the digital educator helps them detect when they might be having a flare-up. Within the app, the patient will find their self-management action plan which gives them instant instruction when it detects that they might be starting to flare up. Over time, Breathe will teach the patient how to become more familiar with exacerbation symptoms and how to work through them. The patient will learn to take action earlier, giving them confidence in knowing when they should and shouldn’t seek urgent care.
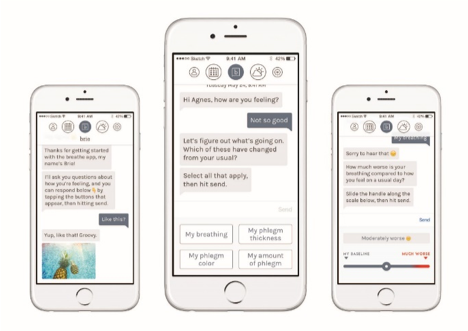
- Exacerbation recommendation based on the Canadian Thoracic Society’s action plan.
- Conversational interface using a chat box that will provide comments and feedback that are digitally programmed into the system.
- System input: Patient identifies their baseline and changes in breathing and sputum.
- Location detection, weather information, and hourly air quality prediction.
Download Breathe: If your patient is an iPhone user and has frequent exacerbations, they can download Breathe today. Search for “Breathe for COPD” or “breathe for Asthma” on the App Store and tap the button. They will be able to sign themselves up right away. Hopefully the app will be available for android users soon.
RESPIRATORY ARTICLE OF INTEREST 1
Lazard AJ, Pikowski J, Horrell L, Ross JC, Noar SM, Sutfin EL. Adolescents’ and young adults’ aesthetics and functionality preferences for online tobacco education. J Cancer Educ. 2019. Available from: https://doi.org/10.1007/s13187-019-1475-4.
Submitted by David Higginson, 3rd year BScN student and Julie Duff Cloutier, Assistant Professor, Laurentian University
Although the use of cigarettes are declining, non-cigarette tobacco products (NCTPs) use is high among young adults and adolescents despite the clear evidence of health risks related to NCTP use. Addressing this involves communicating accurate information to adolescents and young adults in a familiar way, on the internet. There is a need for user friendly mobile apps and websites that convey accurate information in an engaging and informative way.
Online tobacco education is a potential solution to discourage use however there is limited information on how online media should look and function. This study aims to address this issue. Using a two-phase qualitative design, researchers examined existing websites and used focus group feedback to guide the design of a new website that discussed the risks of cigarillos, water pipe (hookah), and e-cigarettes. The focus groups consisted of four 90-minute sessions with 8-11 participants (n=39) for both adolescents (16-17 years old) and young adults (18-26 years old). Groups were separated into tobacco users and susceptible non-users. In phase one, focus groups assessed and expressed opinions regarding aesthetics and functionality of the following websites: therealcost.com, thetruth.com, and stillblowingsmoke.org. Phase one results indicated the importance of layout, font/text presentation, colour, visual tone, imagery/information visualization and social media. Results from phase one guided phase two, which involved the design of a NCTPs education website (suckedin.net) that was reviewed by usability interviews (n=16) with participants from phase one. The collective results indicate the need for responsive designs, uncluttered layouts, easy to navigate interfaces, limited colour variety, and the need for important information to be included instead of dramatic facts and images that may have misconstrued meanings. The findings provide guidelines for online tobacco education to increase engagement among adolescents.
RESPIRATORY ARTICLE OF INTEREST 2
Anderson, R. P, & Zechar, K. Lung injury from inhaling butane hash oil mimics pneumonia. Respiratory Medicine Case Reports. 2019; 26:171-173. Available from: doi:10.1016/j.rmcr.2019.01.002
Submitted by Emily Smith, 3rd year BScN student and Julie Duff Cloutier, Assistant Professor, Laurentian University
“Dabbing” is becoming an increasingly popular form of consuming tetrahydrocannabinol (THC) that utilizes Butane Hash Oil (BHO), an extraction of dried cannabis containing high levels of butane and terpene by-products. BHO is left as a waxy substance that is heated, vaporized and inhaled, and contains up to 75% of THC, compared to 5-20% THC in conventional smoked cannabis.
The authors reviewed a case of a young 18-year-old female presenting to the emergency department (ED) with pneumonia-like symptoms; shortness of breath for 3-4 days, oxygen saturation of 79% on room air. Her condition did not respond to bronchodilators, steroids or supplemental oxygen therapy. Medical history revealed a 1-pack year smoking history and daily BHO use. She was diagnosed with severe pneumonitis with acute hypoxic respiratory failure, secondary BHO inhalation. The authors suggested that the patient developed an acute lung injury after heating the nail to a temperature above 900o F. It is likely that pulmonary irritants including Methacrolein, Benzene and hot vapour were released at this temperature.
The only other literature on lung injury from inhaling BHO located was of a case with a 19-year-old male in 2016 diagnosed with severe pneumonitis after inhalation of BHO. Similarities in the case were highlighted: young patient with no comorbidities, rare tobacco use, daily THC, BHO approximately 1-week prior to ED presentation, hypoxic respiratory failure, clinical improvement with steroids.
Due to its high percentage of THC, “dabbing” is becoming increasingly popular. The authors proposed that lung injury due to BHO inhalation should be considered with a history of marijuana related drug use when witnessing a pneumonia-like presentation. The authors concluded that further exploration of the topic is required due to the unknown short- and long-term effects of BHO use.
RESPIRATORY ARTICLE OF INTEREST 3
Martínez C, Baena A, Castellano Y, Fu M, Margalef M, Tigova O, Feliu A, Larousse K, Galimany J, Puig M, Bueno A, Lopez A, Fernández E. Prevalence and determinants of tobacco, e-cigarettes, and cannabis use among nursing students: A multicenter cross-sectional study. Nurse Educ Today. 2019; 74:61–68. Available from: https://doi.org/10.1016/j.nedt.2018.11.018
Nurses make up the largest group of healthcare providers (HCP) that are often visible to the public. In general, nurses who smoke are less likely to initiate smoking cessation with clients. As such, nursing students hold potential as future HCP to have a role in delivering smoking cessation.
This study examined the prevalence and determinants of tobacco product, cannabis and e-cigarette use in nursing students through a cross sectional multicenter study within 15 nursing schools in Catalonia, Spain. Data collection involved an anonymous self-administered questionnaires (N=4381). The authors calculated the prevalence, odd ratios and confidence levels using a multilevel logistic regression model. Prevalence of cigarette smoking was 29.7% and was 11.5% for cannabis use of all students. Men, and those who were older than 25, were more likely to be smokers (cigarettes and cannabis) than women
Reasons for relapse following cessation included lack of social support, withdrawal symptoms, and the idea that smoking could be controlled. Identified reasons for continued smoking included pleasurable, de-stress, not able to quit, and other smokers in social environment. The authors made it clear that smoking cessation for nursing students must include both a psychological angle, to address stress and social factors, and a pharmacological angle, to address withdrawal. Authors also recommended that cessation programs target younger nursing students as their addiction levels may consolidate along their education.
It is hoped that successful smoking cessation for nursing students will likely result in future nursing staff more willing to support clients in smoking cessation.

Breathe!Bash
Submitted by Peter Glazier, Vice President, Marketing, Development and Public Affairs,
the Lung Health Foundation – Ontario
Each year, our partners in industry and government, our donors, volunteers and Breathing Ambassadors, and the members of our professional societies, come together on one special evening…an evening to celebrate research excellence, to network and meet new friends, and to be inspired by some truly remarkable stories.
Celebrating its 10th anniversary, this year’s Breathe! Bash on March 28, 2019 completely lived up to expectations…and then some!
We shook it up, gave it a shot of adrenaline, and made Breathe! something truly special this year.
Guiding our guests through an amazing evening that put a focus on the breathing breakthroughs that this event has made possible over the past ten years was our emcee, the funny, heart-wrenchingly honest, and brilliant Jeremie Saunders…this year, with his whole Sickboy crew in tow, Brian Stever and Taylor MacGillivary. If you’re not familiar with the Sickboy podcast series, do yourself a favour and check it out!
As always, we were pleased to present our annual TLA-Pfizer Canada Research Award, established to support outstanding investigative studies in the field of infectious lung disease. This year’s well-deserved winner was Dr. Jim Sun.
We also announced our new TLA-Tetra Bio-Pharma Cannabis Research Awards to support ground breaking work on the impact of cannabis on the lungs, and the role of medical cannabis in the treatment of chronic lung disease. This year’s winners were Dr. Tetyana Kendzerska, Dr. Nicholas Vozoris and Dr. Jeremy Hirota.
We also heard from one of our incredible Breathing Ambassadors, Bob Huget, were treated to some amazing food courtesy of MasterChef Canada finalist Chef Michael G, and entertained by the wonderful musician, Jesse Weber. And there was a donut wall!
Whew!
I think it’s an understatement to say that we all went home last night a little more inspired and a little more thankful for all that life has given us.
It truly was an amazing experience.
An event like this doesn’t come together without a strong and talented team, though. A sincere note of thanks and appreciation to everyone that gave their all to making this year’s event the best yet…Cristina, Daniella, Hayley, Kait, Peter, Vero…and, of course, Amy, Donna and Monica for their leadership and vision, and for beautifully orchestrating such an amazing and memorable event. Thanks to their tireless efforts, we completely blew past our goal, raising more than $170,000 (!!!) for life-saving lung research, taking us one step further in creating the breathing breakthroughs of tomorrow.
Mark your calendars for March 26 and don’t miss Breathe! 2020!
WAYS TO GET INVOLVED
Joining an ORCS Committee is a great way to get involved!
Provincial Committee
The Provincial Committee provides leadership to the ORCS and is comprised of the ORCS Chair, a Chair-Elect or Past Chair in alternate years, the Chairs of the five standing committees, the Chairs of the regional planning committees and a member of the Lung Health Foundation Board of Directors.
Editorial Board
Produce an electronic publication for the Ontario Respiratory Care Society (ORCS) members; provide academic content for the publication.
Respiratory Health Educators Interest Group (RHEIG)
Provide respiratory education and a half-day session at the Better Breathing Conference; provide patient education content for the ORCS publication.
Membership Engagement Committee
Recruit and build membership for the Society.
Education Committee
Session planning for the Better Breathing Conference.
Research and Fellowship Committee
Manage the funding process including Grant and Fellowship application review and funding allocation.
Regional Planning Committees
Regional Planning Committees plan educational events in their respective regions. The Regions include:
Northeastern Region
Northwestern Region
Eastern Region
Central Region
Western Region
To find out more, or to join one of these Committees, contact the OTS/ORCS Coordinator,
Natalie Bennett, nbennett@lungontario.ca
UPCOMING EVENT LISTINGS
July 11, 2019
Spirometry Interpretation Workshop
Belleville
CFPC Mainpro+ Certified
Funded by Ministry of Health and Long Term Care
Registration Coming Soon
September 12, 2019
Spirometry Interpretation Workshop
Ottawa
CFPC Mainpro+ Certified
Funded by Ministry of Health and Long Term Care
Registration Coming Soon
September 13, 2019
Asthma Action Plan Workshop
NPAO Conference
Sheraton Centre Toronto
Funded by Ministry of Health and Long Term Care
More Information (https://npao.org/events-education/npao-conference/)
September 14, 2019
Spirometry Interpretation Workshop
PFT Symposium
Novotel Ottawa
Funded by Ministry of Health and Long Term Care
Register here (www.eventbrite.ca/e/pulmonary-function-testing-symposium-2019-registration-60277112466)
September 26, 2019
Breathing Inspired
ORCS Western Region Evening Seminar
Fanshawe College London
Registration Coming Soon
October 10, 2019
Asthma COPD Overlap Workshop
HHS Respiratory Therapy Educational Retreat
Carmen’s Banquet Centre Hamilton
Funded by Ministry of Health and Long Term Care
More Information (http://events.hamiltonhealth.ca/site/TR?fr_id=1980&pg=entry)
October 27, 2019
COPD – Acute Exacerbation and End-of-Life Workshop
Practical Pearls in Long-Term Care Conference
Sheraton Centre Toronto
Funded by Ministry of Health and Long Term Care
More Information (https://www.oltcc.ca/annual-conference/)
October 29, 2019
Breathing Inspired
ORCS Eastern Region Evening Seminar
Italo-Canadian Club Kingston
Registration Coming Soon
October 2019
Breathing Inspired:
ORCS North Eastern Region Seminar
Sudbury
Details and Registration Coming Soon
October 30, 2019
COPD Workshop
Southlake Regional Health Centre Newmarket
CFPC Mainpro+ Certified
Funded by Ministry of Health and Long Term Care
Registration Coming Soon
November 7, 2019
Breathing Inspired: COPD Rehabilitation – Communicating the Diagnosis and Prognosis
ORCS South Central Region Evening Seminar
Hamilton
Registration Coming Soon
RESPTREC® Workshops
Asthma: Toronto September 26-27, 2019
Ottawa October 25-26, 2019
COPD: Toronto October 5-6, 2019
Education: Toronto September 28-29, 2019
Ottawa October 27-28, 2019
Spirometry: Toronto October 4, 2019
November 9, 2019
Steeltown Stair Climb
http://support.on.lung.ca/site/TR/StepUpampBreathe/StepUpClimbEvent?fr_id=1230&pg=entry
EDITORIAL Committee
CO-CHAIRS
Yvonne Drasovean, RRT
Lorelei Samis, BScPT
MEMBERS
Jocelyn Carr, BScPT, MSc
Julie Duff Cloutier, RN, MSc, CAE
Yvonne Drasovean, RRT
Elizabeth Gartner, BScOT
Lawrence Jackson, BScPhm
Rachel McLay, HBSc (Kinesiology)
Shirley Quach, HBsc, RRT
Priscila Robles, BScPT, MSc, PhD
Lily Spanjevic, RN, BScN, MN, GNC(C), CRN(C), CMSN(C)
CHAIR, ONTARIO RESPIRATORY CARE SOCIETY
Miriam Freymond Turnbull, MBA, RRT, COPD Ed.
Vice President & GM | ProResp Inc.
PRESIDENT & CEO, THE LUNG HEALTH FOUNDATION
George Habib, BA, BEd, CAE
SENIOR DIRECTOR, PROGRAMS & SERVICES
Christina Sperling, MScCH, BKin, RRT
OTS/ORCS Coordinator
Natalie Bennett
An official publication of the Ontario Respiratory Care Society, a section of the Lung Health Foundation.
RHEIG Committee
CO-CHAIRS
Jane Lindsay, BScPT
Lorelei Samis, BScPT
MEMBERS
Aisha Balasubramaniam, MPH, BSc, RRT, CRE
Geetika Bhargava, BHSc, RRT, CRE
Michael Callihoo, RRT, CRE
Rose-Marie Dolinar, RN(EC), MScN, PhD student
Kitty Seager, CRE, CTE, RPN
Sylvia Sirarajahkumar, HBSc, BScPharm, ACPR
Maria Willms, RN, CRE