Prior to 2020, the Lung Health Foundation operated as the Ontario Lung Association. Enjoy this content from our archives.
An official publication of the Ontario Respiratory Care Society, a section of The Lung Health Foundation
Update on Respiratory Health, Research and Education is a publication of the Ontario Respiratory Care Society, a section of the Lung Health Foundation. Update is published three times per year and includes peer-reviewed original articles, clinical practice tools, health news, and communications between the ORCS and its membership.
Discounted Liability Insurance through your ORCS Membership is here!
A big thank you to all of you who took our recent ORCS Survey! 45% of you who responded said that you would be interested in benefiting from Liability Insurance through your ORCS Membership.
We’ve listened, and are pleased to offer you Liability Insurance through JD Smith that includes:
- $2,000,000 Errors and Omissions Insurance – $75.00 per year
- $5,000,000 Errors and Omissions Insurance – $150.00 per year
- Group Health Insurance starting at $89.00 per month
- Group Travel Insurance starting at $2.00 per day
- Group Office Insurance from $395.00 including a 30% Discount
- Access to FREE legal consultation
These rates and coverage are competitive with other societies, but with an ORCS membership costing less, you come out ahead!
AND…
Other perks we’ve secured include a discount with Park N’ Fly as well as up to 40% off GoodLife fitness memberships for you and your family! We’ll be working over the coming months to secure additional benefits to the portfolio of savings. Information on how to take advantage of these savings programs will be arriving to your inbox over the coming weeks. Stay tuned!

CHAIR’S MESSAGE
The summer months are a time to slow down a little and recharge our batteries before the busyness of the fall is upon us. It is also a time to reflect on the months that led up to summer and all of the work that occurred. This year, there has been a lot of change, and change can be challenging. However, it also offers the opportunity to evaluate current state and push things forward. The membership of the Ontario Respiratory Care Society (ORCS) is extremely important to the Lung Health Foundation and to myself. Our collaborative goal is to ensure that members feel that they are part of a community of practice that is engaging and valuable.
Over the summer, the Lung Health Foundation, along with the ORCS Research and Fellowship Committee had the pleasure of notifying the recipients of the ORCS Research Grants and Fellowship Awards. These grants and awards are distributed to respiratory healthcare professionals that are committed to advancing respiratory care across Ontario. This year we are pleased to congratulate the following recipients of the Research Grant funds: Darlene Reid, Sunita Mathur and Dina Brooks; and the recipients of the Fellowship Awards: Christina McMillan-Boyles, Erin Miller, Kenneth Wu, and Shirley Quach. We are thrilled to have such talented and dedicated individuals working to improve the lung health of all Ontarians!
Over the last few months our Regional Planning Committees have been very busy planning six educational events in six different areas across the province. We are excited to have exceptional speakers come out to share their expertise with members and students eager to build their knowledge. Topics scheduled include: The Truth about Cigarettes, Vaping and Marijuana in London, Lung Cancer Screening in Northern Ontario in Sudbury, The Role of the Microbiome in Allergies and Asthma in Kingston, COPD and Pulmonary Rehabilitation in Hamilton, and Pulmonary Rehabilitation in Toronto.
The Lung Health Foundation is very excited to introduce Jennifer Noble, our new Senior Manager, Member Engagement for both the ORCS and Ontario Thoracic Society (OTS). Jennifer comes to the organization on September 12th, 2019 and brings with her years of experience in providing operational support and leadership to members. She is committed to proactively engaging members throughout the lifecycle of their membership, understanding their needs and ensuring members’ views are a central part of strategy development and operational plans. Jennifer is looking forward to forging solid relationships with ORCS members and developing our community further into the future.
We want you to know that we heard you in our recent survey and are pleased to have finalized a comprehensive insurance offering that will include liability, home and vehicle insurance, travel and health insurance options. More information will be arriving to your inbox soon.
Finally, don’t forget that Better Breathing 2020 is coming – January 23-25, 2020! This is one of Canada’s leading respiratory conferences, and is hosted collaboratively by the Ontario Thoracic Society (OTS), the Ontario Respiratory Care Society (ORCS) and the Lung Health Foundation. We look forward to seeing you there.
Respectfully submitted,
Miriam Freymond Turnbull, MBA, RRT
Chair, Ontario Respiratory Care Society

EDITOR’S MESSAGE
Over the past year, we have seen changes in our healthcare system, our post-secondary healthcare education, and changes at the Lung Health Foundation. Change can be hard, but it can also be an opportunity for renewal. It is a chance to broaden one’s horizons, to learn about new treatments, to gain new information to help our patients achieve optimum health, to find new ways to interact with our colleagues, and to discover new ways to mentor our students. Through this sea of change, the Editorial Board of Update on Respiratory Health, Research, and Education remains committed to bringing you interesting and up to date
information in the area of respiratory health through our online publication. We are fortunate to be working with some new and dynamic staff at the OLA who are dedicated to helping us continue to achieve our goals.
One thing that has not changed is that another amazing Better Breathing Conference is on the horizon. We hope to see many of you from January 23 to 25, 2020 in Toronto for this wonderful learning and networking experience. See you there!
Sincerely,
Lorelei Samis PT, COPD Educator
Co-chair Editorial Board
Co-chair RHEIG Executive Team
Inter-Professional Preceptorship
By: Dr. Christine Griffith, MHA, EdD, Associate Dean, School of Health Sciences, Fanshawe College, London, Ontario
When Health Practitioners Become Educators: Identities and the Challenges of Transition
Introduction
Educational institutions offering health care programs depend on the willingness of expert clinicians passionate about their profession to join them in preparing the next generations of health care professionals (HCP). In particular, in programs preparing students to become members of regulated health professions, courses considered core to the disciplines must be taught by individuals with a current license to practice, who can bring to their classrooms experience and in-depth knowledge of the discipline. Candidates for full-time professor positions are generally expected to have demonstrated expertise and leadership as practitioners, as well as competence in teaching in a part-time capacity. They are also expected to maintain their license to practice. Health care educators therefore adopt a dual identity, which is that of educator and of a member of a regulated health profession with two independent sets of expectations and obligations. Read More.

Immunization
By: Kait Allen, Content Manager, Lung Health Foundation
Influenza Immunization and the Health of Seniors: where we are now, and where we need to be
How can we encourage more Canadians to protect themselves against breathing breakdowns?
In Ontario alone, seasonal influenza vaccines eliminate the need for more than 200,000 visits to doctors’ offices, avert approximately 30,000 visits to hospital emergency departments, and prevent approximately 300 deaths each year.1
With stats like these, it is clear that immunization against the flu has a positive effect on people of all ages. But current national and provincial vaccination rates remain far from ideal, despite the human and economic toll of infectious diseases like the flu.
The Lung Health Foundation and its medical societies are working to spread the message that getting vaccinated is one of the most important things that people of all ages can do to protect their lung health, especially if they are at higher risk of serious complications due to their age. Read More

Tobacco Reduction in Youth Partnerships: Supporting Youth to Decrease Smoking Rates in Northwestern Ontario
By: Kellie Milani, Youth Development Specialist, Northwest Tobacco Control Area Network
Thunder Bay District Health Unit, 999 Balmoral Street
Smoking rates among youth in Northwestern Ontario are higher than the provincial average. Compared to youth in other regions of Ontario, it is not unusual for youth in Northwestern Ontario to face other health challenges, such as higher rates of alcohol, cannabis and other substance use, physical inactivity and poor mental health. Growing up in rural and remote communities is common in Northwestern Ontario. This can contribute to these health challenges because often youth have fewer opportunities to participate in structured recreation, sports and arts activities outside of the school day, which support healthy recreation and social connection. Other barriers such as lack of transportation and funding also decrease youth access to services and opportunities. Northwestern Ontario is home to the highest proportion of Indigenous people in Canada, and although the smoking rate for Indigenous youth has decreased over the years, the evidence still shows that they smoke at a higher rate and have an earlier age of initiation than their non-Indigenous peers. Read More

TIN THE SPOTLIGHT – Darlene Reid
Written by Chris Haromy at the Lung Health Foundation
Darlene Reid has proven to be a very motivated and inspiring individual. After receiving her Bachelor of Medical Rehabilitation (PT) from the University of Manitoba, she chose to continue her studies and went on to complete her PhD at the University of British Columbia in 1988. Dr. Reid was a Professor in the Department of Physical Therapy at the University of British Columbia for many years, where she chaired the Research Graduate Programs in Rehabilitation Sciences and was responsible for growing the program significantly. In 2014/2015 Dr. Reid moved across the country to Toronto to become the Chair of the Department of Physical Therapy. Read More
TOOL BOX

Spirometry Interpretation Guide
Submitted by Aisha Balasubramaniam, RRT, CRE, MPH
The Canadian Thoracic Society (CTS) clinical guidelines for asthma and chronic obstructive pulmonary disease (COPD) recommend the use of spirometry for the diagnosis of these diseases.1 Due to the burden of asthma and COPD, most individuals with these diseases are diagnosed in primary care. In Ontario, physicians and nurse practitioners can interpret spirometry however; few of them have had specific training in the analysis of spirometry data.
The Lung Health Foundation’s Provider Education Program (PEP) develops and implements evidence-based continuing medical education programs to promote the implementation of CTS guidelines. They facilitate spirometry interpretation workshops and provide online learning modules for training purposes. One of their learning resources is the Obstruction/Restriction Algorithm developed by Dr. Josiah B. Lowry in 1998 as a guide to interpret spirometry for primary care providers.2 Based on student evaluations, this was a valuable tool for understanding and performing spirometry interpretation. However, this tool does not reflect the latest research and current CTS respiratory guidelines.
The PEP steering committee invited leading researchers, respirologists and primary care providers to join a working group to revise the Obstruction/Restriction algorithm to ensure its continued use by primary health-care providers. The revision process took two years and included feedback from various expert groups in Ontario, resulting in the establishment of a new Spirometry Interpretation Guide, Version 2018.3,4 The Guide is a great tool aimed to assist with accurate interpretation of spirometry testing conducted in primary care and has received endorsement by the Ontario Thoracic Society for use across Ontario.3
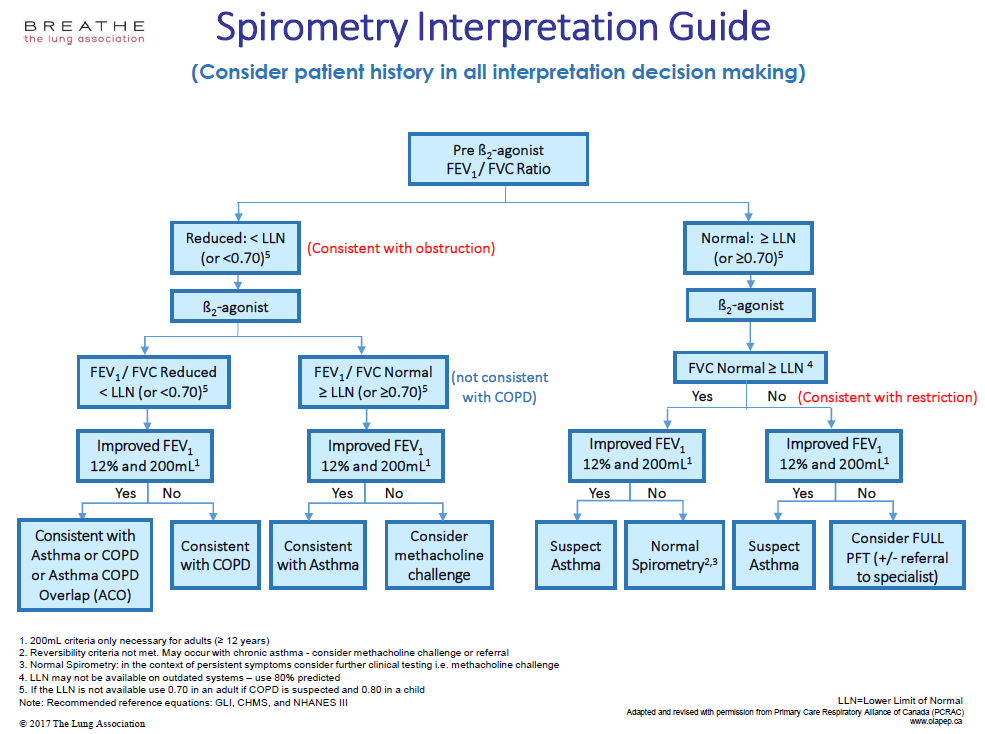
The Guide is in a table format and provides clear instructions to discern between asthma, COPD, asthma COPD overlap (ACO), or the presence of restrictive lung disease. In addition, other recommended tests are provided to better direct diagnosis. It is crucial to consider patient history and clinical presentation in all interpretation decision making.
RESPIRATORY ARTICLE OF INTEREST 1
Turcotte D, Woskie S, Gore R, Chaves E, Adejumo K. Asthma, COPD, and home environments. Ann Allergy Asthma Immun. 2019; 122(1). 486-491.
Summary by David Higginson, 4th year BScN Student and Julie Duff Cloutier, RN, MSc Laurentian University School of Nursing
Asthma in adults 65 years and older is prevalent and often underdiagnosed, with older adults being more sensitive to poor indoor air quality. This study is a response to the lack of evidence on home environmental interventions for older adult patients with diagnosed asthma. An observational study of adults (62 years and older) with asthma in Lowell Massachusetts was conducted to assess the health and environmental conditions that may pose barriers to effectively managing this disease. The sample population consisted of 93 adults from 90 households, who were diagnosed with asthma by a physician, resided in public or private subsidized housing and were prominently of Hispanic ethnicity.
Community health workers (CHW) assessed health outcomes with multiple metrics of respiratory health and quality of life. The participants were assessed initially and one year later after implementing various interventions. Follow up assessments were done at the same time of year as the initial assessments to avoid seasonal influence on health measure outcomes.
Interventional plans were individualized for each participant based on information gathered from asthma trigger activity and exposure questionnaires performed by a CHW and an Environmental Assessor (EA). Interventions included pest management, mattress encasements, cleaning supplies and structural interventions as well as education.
The study found that at final assessment ER visits had decreased by 37.5% and asthma related doctor visits decreased by 50%, asthma related hospitalization decreased by 43.8% and antibiotic treatment for chest infection decreased by 46.6%.
Multifaceted environmental interventions in homes of older adults with asthma could reduce doctor visits and improve health, as well as reduce health care costs. The lack of a control group in this study is a limitation. Further research relative to the implementation of interventions in homes of older adults with asthma is needed to guide treatment of the study population.
RESPIRATORY ARTICLE OF INTEREST 2
Gupta S, Cheung V, Kastner M, Straus S, Kaplan A, Boulet L, Sale J. Patient preferences for a touch screen tablet-based asthma questionnaire. J Asthma. 2019; 56(7): 771-781.
Submitted by Julie Duff Cloutier, RN, MSc, Laurentian University School of Nursing
Assessment of asthma control and provision of asthma action plans are important components of asthma management but are often not completed in practice due to time constraints. Guidelines recommend assessment of asthma control at every visit and again, it is recommended that all patients have an individualized asthma action plan. It has been suggested that patient questionnaires may improve process and efficiency of care and the administration of questionnaires through tablet devices is feasible. To address this issue, the authors designed an electronic asthma questionnaire that was completed by patients in the waiting room to collect some of this important information. Collection of some of this important information while patients are waiting may contribute to improved asthma management as it addresses the issue of time constraints in practice.
A questionnaire prototype was created based on evidence and rapid cycle design (semi-structured focus group testing, modifications, re-testing) with asthma patients aged 16 and older. Sample size was 20 across five focus groups. Qualitative and quantitative measures were used. Content related themes included; comprehensibility and information collection (subthemes: personal symptoms, control, medications). Average completion time was 12 minutes and summative Likert scale responses suggested high levels of question comprehension and confidence in answers.
These study results provide insight into one way to formulate and present asthma-related content in an electronic form. Such questionnaires may improve efficiency of data collection and better enable assessment of asthma control and medication use and asthma action plans.
RESPIRATORY ARTICLE OF INTEREST 3
Bass B, Lake E, Elvy C, Fodemesi S, Iacoe M, Mazik E, Brooks D, Lee A. Smoking-related stigma expressed by physiotherapists toward individuals with lung disease. 2018; 70(1). Available from: 10.3138/ptc.2016-98.
Submitted by: Julie Duff Cloutier, RN, MSc, Laurentian University School of Nursing
The purpose of this study was to determine the extent and nature of stigma exhibited by a sample of Canadian cardiorespiratory physiotherapists toward people with lung disease who had a smoking history. Health professionals may express two types of stigma: explicit and implicit. Explicit stigma is described as overt, or conscious, controllable attitudes toward an individual or group and implicit stigma is described as subtle or unconscious attitudes. As a result, individuals may harbour negative attitudes that can affect their actions without them being aware of it. Either type of stigma can influence the quality of care they deliver.
A quantitative online survey was distributed to Canadian cardiorespiratory physiotherapists and an anti-smoking attitudes questionnaire was used to measure explicit stigma. Two case studies were used to measure implicit stigma: one case described an individual with Chronic Obstructive Pulmonary Disease (COPD) with a smoking history and one case described an individual with COPD without a smoking history.
Most respondents (n=50) exhibited some degree of explicit stigma; 56% exhibited mild explicit stigma and the remainder, moderate to severe explicit stigma. Implicit stigma was not significantly different between the two cases. Findings suggest that a proportion of Canadian cardiorespiratory physiotherapists appear to demonstrate a mild degree of explicit stigma towards individuals with lung disease and a smoking history. However, there is no evidence that it has any effect on treatment choices based on the hypothetical case studies. Further work is needed to examine the implicit stigma on treating patients with lung disease.

Lana Biro, BSc, RRT, CRE
Curriculum Developer, Provider Education Program, Lung Health Foundation

Laura Seed Laura Seed, MSc, RCPT(p) Registered Cardio-Pulmonary Technologist President, CACPT
Spirometry Certification to Improve Tester’s Skills and Test Quality
The Canadian Association of Cardio-Pulmonary Technologists (CACPT) is now happy to offer Spirometry Certification to improve the skills and quality of Spirometry testing for those performing Spirometry testing in a hospital setting as well as any other facility such as doctors’ offices, family health teams, and research labs. This will allow those involved in Spirometry Testing to deliver quality care by accurately diagnosing, treating and managing the individual with respiratory disease. It will also provide researchers who require spirometry data with statistical confidence to help prove their hypothesis.
CACPT offers Certification to all eligible allied health professionals: RPNs, RNs, Nurse Practitioners, Pharmacists, or those approved by the CACPT Education Committee. Individuals seeking Certification must also be employed in a facility that routinely conducts Spirometry tests and meet Spirometry Testing Experience guidelines.
The Spirometry Certification Exam:
The National Spirometry Certification examination is a 2-hour, online multiple-choice exam. The exam will have sittings across Canada at specific proctored testing centers. The CACPT has contracted the professional services of the Canadian Board of Respiratory Care (CBRC) and Yardstick to compile, administer, and score the Spirometry Certification Examination.
CACPT offered the first sitting of the exam on September 30, 2019. Please check www.cacpt.ca for the next sitting of the Spirometry Certification exam.
Why Certification?
- Spirometry is the most reliable way to help diagnose lung disease and assess disease progression and response to treatments.
- Poorly performed spirometry greatly increases the risk of misinterpretation of results, misdiagnosis and incorrect treatment.
- Spirometry Certification provides an objective assessment of knowledge and competency for individuals who have completed a spirometry training course and maintain competency at 3 year intervals.
Spirometry Certification will lead to:
- Greater confidence in results.
- Higher quality of testing.
- Increased number of successful tests.
- Improved understanding of the impact of testing procedures, choice of predicted values, formatting of results.
- Strong knowledge of Quality Control requirements and procedures.
- Improvements in patient care.
Criteria for Eligibility to Challenge the Exam:
To challenge the CACPT National Spirometry Certification, you must meet the following criteria:
EITHER
- Have completed a Spirometry course approved by CACPT within the past thirty-six (36) months.
OR
- Have received at least three months of on the job Spirometry Testing Training and submitted seven (7) Spirometry Examples performed by the applicant under the supervision of a qualified preceptor. The qualified preceptor must be a physician or Registered Respiratory Therapist (RRT) or Registered Cardiopulmonary Function Technologist (RCPT(P)) registered with the CACPT, or allied health professional who are currently active in Spirometry testing.
For more information on Spirometry Certification examination or to submit an application,
Visit Canadian Association of Cardio-Pulmonary Technologists website www.cacpt.ca
WAYS TO GET INVOLVED
Joining an ORCS Committee is a great way to get involved! Read More
CO-CHAIRS
Yvonne Drasovean, RRT
Lorelei Samis, BScPT
MEMBERS
Jocelyn Carr, BScPT, MSc
Julie Duff Cloutier, RN, MSc, CAE
Yvonne Drasovean, RRT
Elizabeth Gartner, BScOT
Lawrence Jackson, BScPhm
Rachel McLay, HBSc (Kinesiology)
Shirley Quach, HBsc, RRT
Priscila Robles, BScPT, MSc, PhD
Lily Spanjevic, RN, BScN, MN, GNC(C), CRN(C), CMSN(C)
CHAIR, ONTARIO RESPIRATORY CARE SOCIETY
Miriam Freymond Turnbull, MBA, RRT, COPD Ed.
Vice President & GM | ProResp Inc.
PRESIDENT & CEO, THE LUNG HEALTH FOUNDATION
George Habib, BA, BEd, CAE
SENIOR DIRECTOR, PROGRAMS & SERVICES
Christina Sperling, MScCH, BKin, RRT
OTS/ORCS Coordinator
Natalie Bennett
RHEIG Committee
CO-CHAIRS
Jane Lindsay, BScPT
Lorelei Samis, BScPT
MEMBERS
Aisha Balasubramaniam, MPH, BSc, RRT, CRE
Geetika Bhargava, BHSc, RRT, CRE
Michael Callihoo, RRT, CRE
Rose-Marie Dolinar, RN(EC), MScN, PhD student
Kitty Seager, CRE, CTE, RPN
Sylvia Sirarajahkumar, HBSc, BScPharm, ACPR
Maria Willms, RN, CRE